By Michelle Shapiro and Nicki Parlitsis | Read Time: 10 Minutes
In this post, we’ll debunk common cholesterol myths, explain the truth about cholesterol, and give you functional nutrition strategies for heart health.
Cholesterol has gotten a really bad rap the past few years, but is it really as “bad” for heart health as we’ve been made to believe? Hint: It’s probably not what you think.
Disclaimer: This is not a substitute for medical advice. This is for educational purposes only.
What is Cholesterol?
Cholesterol is a waxy, fat-like substance made by the liver. It is an essential component of every cell in the body, serving multiple functions:
- Contributes to the structure of the cell
- Necessary component in the formation of Vitamin D and sex hormones (estrogen, testosterone, progesterone)
- Helps make bile acids that assist in absorption of fats & fat-soluble vitamins (Vitamins A, D, E, and K)

What does cholesterol do?
Cholesterol is transported through the blood inside different lipoproteins, some of which are listed below:
- LDL-C – LDL cholesterol carries cholesterol from the liver to the body’s cells, tissues, and arteries. This is typically known as the “bad” cholesterol, but it’s important to know that different types of LDL can impact the body in different ways.
- LDL-A – LDL-A particles are large & fluffy LDL particles. They are harmless as they are much less likely to be oxidized by free radicals
- LDL-B – LDL-B particles are smaller, more dense LDL particles. They can be more harmful as they are more likely to become oxidized and stick to arterial walls, increasing the risk of atherosclerosis and heart disease. Luckily, it is possible to shift from a pattern of LDL-B (more harmful) toward a pattern of LDL-A (less harmful) through dietary and lifestyle changes.
- HDL – HDL picks up excess LDL cholesterol from tissues and arteries, bringing it back to the liver to be removed from the body (think: More HDL is helpful because it can help clear out the more harmful particles)
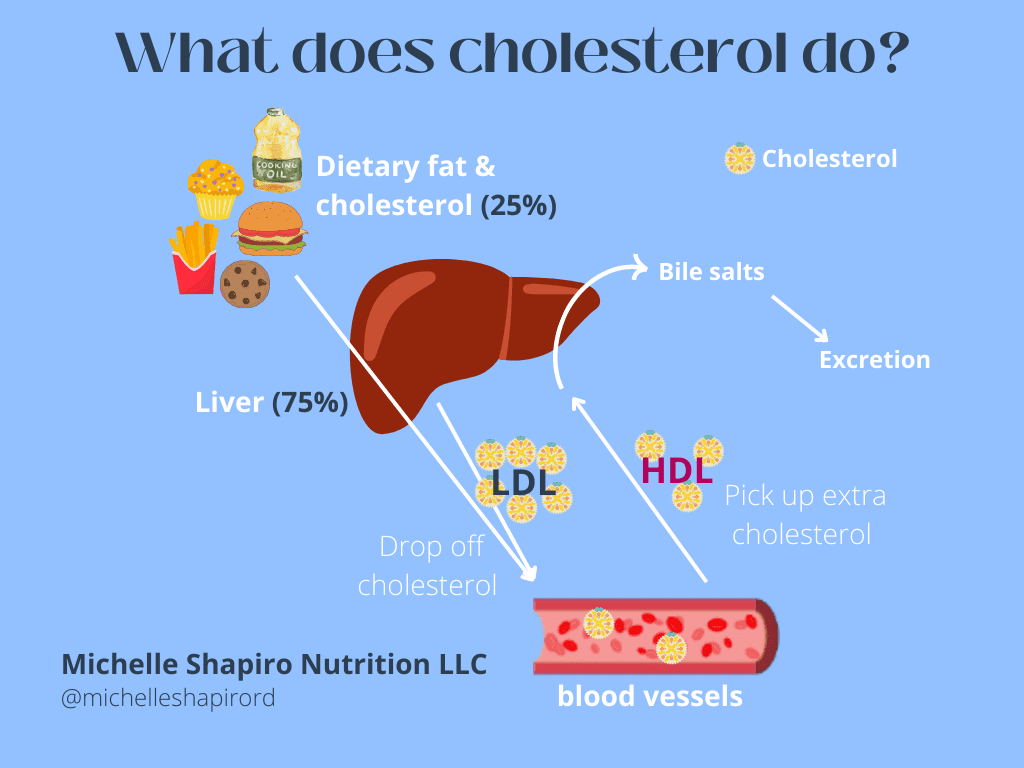
How do we make cholesterol?
Contrary to what we’ve been told in the media, only about 20-25% of the cholesterol in our body comes from what we eat (in most people). About 80% of the cholesterol in the body is actually produced by the liver. Certain conditions may cause the liver to make more cholesterol, including:
- Insulin resistance
- Metabolic syndrome
- Adrenal dysfunction & stress
- Genetics (Familial Hypercholesterolemia – high cholesterol that runs in the family)
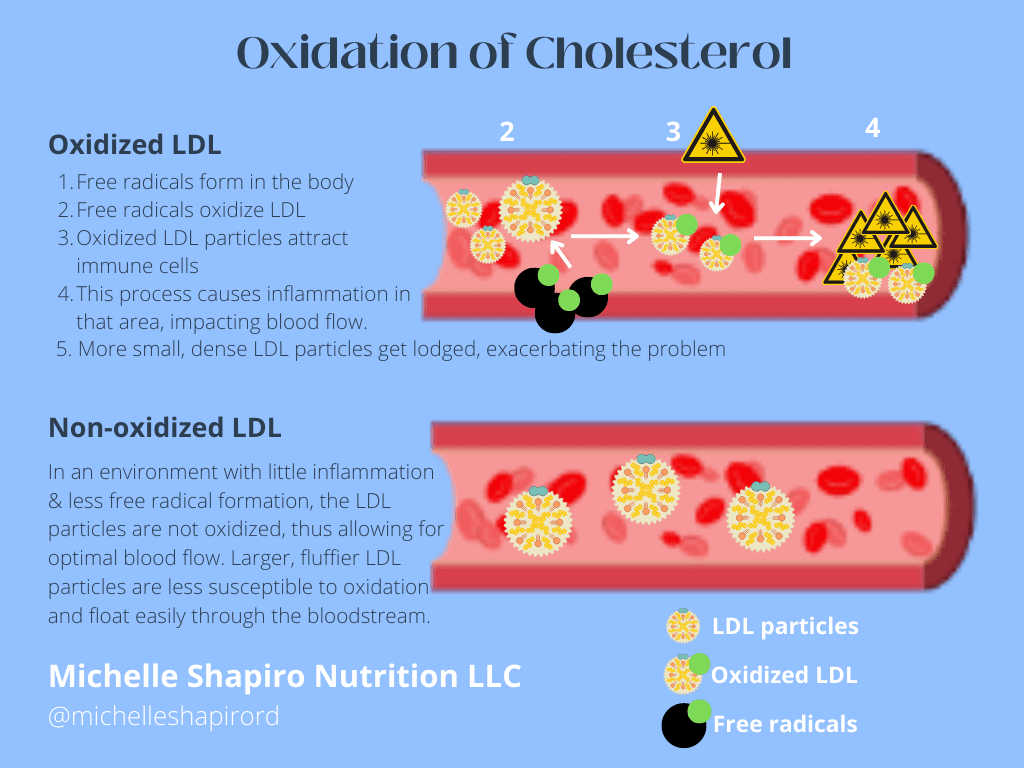
When is cholesterol actually a problem?
Certain types of cholesterol (think: Small, dense LDL particles) are more susceptible to oxidation by free radicals in the body. It’s this oxidation that can lead to further inflammation and plaque formation in the arteries, restricting blood flow and contributing to heart disease. This is why it’s not necessarily “bad” to have high LDL cholesterol; however, we want to reduce the amount of LDL-B (small, dense LDL that is prone to oxidation). Furthermore, it’s also not necessarily the cholesterol itself that is causing heart disease. It’s this oxidation that causes problems; therefore, we want to reduce the opportunities for oxidation.
Free radicals contribute to a host of issues in the body, one of which is the oxidation of LDL cholesterol. These free radicals can be generated from:
- Excess PUFAs (vegetable oils)
- Smoking cigarettes
- Processed foods (margarines, fast foods, commercially fried foods, commercially baked goods)
- Immune cell activation
- Infection
- Cancer
- Mental stress
- Ageing
- Ischemia
Below is a graphic detailing the process of how oxidation can contribute to atherosclerosis (clogged arteries).
Debunking Cholesterol Myths
Myth 1: Cholesterol is bad
Truth: Cholesterol is a necessary component of every cell in the body
Cholesterol supports the structure of cells, forms the basis of Vitamin D and other sex hormones, and helps aid in the absorption of fats and fat-soluble vitamins. Different types of cholesterol can have different impacts on the body (i.e. LDL, HDL, Small vs. large particle size).
Myth 2: High cholesterol levels in the blood are caused by cholesterol in the diet
Truth: 20-25% of the cholesterol in our blood comes from our diet; 75-80% of cholesterol is made by the liver
Certain conditions may influence the liver to produce more cholesterol:
- Insulin resistance and Type II Diabetes
- Metabolic syndrome
- Adrenal dysfunction and stress
- Genetics*
*About 15-25% of the population are hyper-responders to dietary cholesterol. This means that based on their genetics, these people may experience an almost 3x greater response to cholesterol through the diet compared to the rest of the population (think: Higher blood cholesterol levels).
Myth 3: High cholesterol = Heart disease
Truth: The oxidation of cholesterol by free radicals in the body and pre-existing inflammation is what causes the most damage to blood vessels, not so much the cholesterol itself.
By examining LDL particles that have been removed from arterial plaques in both humans and animals, it has been apparent that these LDL cholesterol particles have all the properties of oxidation. Thus, we can conclude that the oxidation of these particles contributed to the clogging of these arteries. Furthermore, there are people that have high LDL cholesterol numbers with no evidence of heart disease. This information is extremely important in disease prevention because it tells us that it’s much more impactful to prevent oxidation and inflammation than the cholesterol itself, as these are both factors in many other chronic diseases as well (in addition to heart disease).
Is your high cholesterol the harmful kind?
So, you’ve been told you have high cholesterol levels (or a family history of heart disease) and your doctor might even be talking about medication. Instead of immediately working to lower cholesterol, it’s helpful to learn if your cholesterol is in fact harmful (and if it needs to be lowered in the first place). Here are some next steps you can take:
1. Ask for additional labs
High cholesterol is NOT the full picture. To evaluate risk for cardiovascular disease (CVD), it can be helpful to request tests for the following:
- Homocysteine – Homocysteine is a marker of inflammation and an independent risk factor for CVD.
- Apolipoprotein A-1 – Apolipoprotein A-1 is a major component of HDL cholesterol. Higher levels are usually a sign of low CVD risk.
- Apolipoprotein B – Apolipoprotein B is a major component of LDL cholesterol. Higher levels are usually a sign of high CVD risk.
- C-reactive protein (CRP) – CRP is another marker of inflammation.
- Ferritin – Ferritin can be a marker of inflammation, oxidative stress, and/or a need for liver support. Higher levels may indicate a higher risk of CVD.
2. Target inflammation instead of animal foods
Heart disease starts with arterial inflammation and LDL-C can be a sign of inflammation. Instead of focusing on cholesterol, we could instead focus more on (often reversible) factors that cause arterial inflammation and ultimately heart disease. Thus, supporting overall health and disease, not just cholesterol.
There is no compelling evidence to suggest that intake of nutrient-dense, organic animal protein correlates with heart disease. Instead of working to lower cholesterol, learn if your cholesterol is in fact harmful (and if it needs to be lowered in the first place).
See our post on 5 Ways to Lower Cholesterol for specific anti-inflammatory tips!
Bottom Line
It’s the oxidation of these cholesterol particles by free radicals & pre-existing inflammation that can cause damage, not so much the cholesterol itself. If your labs indicate high cholesterol, have an ongoing discussion with your doctor about further testing and finding the root cause.
Looking for a natural way to support heart health?
By working with one of our Registered Dietitian Nutritionists at Michelle Shapiro Nutrition LLC, you will receive personalized recommendations and one-on-one nutritional counseling to help you reach attainable goals in a way that fits your lifestyle.
[…] we discussed in a previous blog post, high cholesterol levels may not be the immediate concern that we once thought they were. […]