Season 3 Episode 2 of Quiet the Diet Podcast with Michelle Shapiro, RD and Nicki Parlitsis, RD
What is the Difference Between Hunger and Appetite, and How to Navigate Cravings with Michelle & Nicki

Understanding appetite is a key aspect of our exploration into functional nutrition and body positivity. Rather than reacting or judging our appetite, we’re encouraged to approach it with curiosity. How can we better understand the signals our body is sending us?
In part one of this two part series on hunger, appetite and cravings, Michelle and Nicki dive into the historical association between appetite and illness, as well as the study of appetite suppressants for weight loss. They explore questions about the effectiveness and safety of decreasing appetite for weight loss and whether genetic factors influence our appetite.
Cravings, too, play a significant role in appetite. Could they be a result of nutrient deficiencies or imbalances? Can certain mental restrictions increase our cravings? How can we navigate cravings without falling into unhealthy patterns?
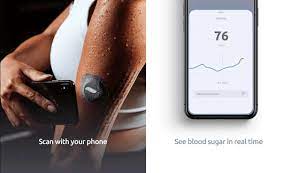
This episode is sponsored by Veri Continuous Glucose Monitor $30 off your order with code VSM-QUIETTHEDIET by clicking HERE
Listen in as Michelle and Nicki debunk myths, separate fact from fiction, and help you develop a healthier approach to your appetite.
They discuss:
- The physiology of hunger and appetite [12:25]
- Leptin hormone and its role in appetite regulation [14:46]
- How food cravings and appetite are influenced by hormones and stress [21:18]
- The underlying causes of food cravings [25:13]
- Relationship between low food access, overeating, and mental obsession [30:40]
- The impact of psychological restriction vs physical restriction [53:05]
- Why we should incorporate an additive mindset vs restrictive thinking [1:05:34]
** Links for the studies referenced are on our Episode Page!
Connect with Nicki:
Follow Nicki on IG @nutrition.nicki
Podcast Links:
Quiet the Diet Podcast Page
Follow the pod on IG
Episode Page (with full transcript!) + Study links
Work with Michelle:
Work 1-on-1 with a functional Registered Dietitian at MSN LLC
8-Week Fitness & Nutrition Guide
Learn more about the practice
Free Resources:
Get started with any of our free guides
Sign up for the Newsletter
Join our FREE membership community!
Connect with Michelle:
Follow the pod on IG
Follow Michelle on IG
Episode Transcript
What is the Difference Between Hunger and Appetite, and How to Navigate Cravings with Michelle & Nicki
Michelle [00:00:01]:
Season three. Season three. We have Nicki back in the house. I’m so excited.
Nicki [00:00:07]:
I’m so excited for season three.
Michelle [00:00:10]:
We’re back. I know this is episode two of season three, but it still feels so new. Season three. It’s so exciting.
Nicki [00:00:16]:
Well, we had a little hiatus, but it was because we were just getting all the juicy stuff together 100%.
Michelle [00:00:22]:
The hiatus was not a break was taken and that we promised. We were still hustling the whole, you know, we always talk about this thing in our practice, Nicki, where we get really into these conversations about different things with clients. And it’s just so funny because the same conversations will keep coming up. And something that’s been coming up a lot for us and in our practices is conversation around appetite, around hunger, around cravings. And really, in previous episodes, in previous seasons, we’ve talked about binge eating from kind of a nervous system standpoint. We’ve talked about cravings from those kind of physiological standpoints. I think what we want to do today is really talk about appetite, hunger and cravings and talk about how they might be impacted from a physical standpoint and talk about how they might be impacted from a physical standpoint and also a mental standpoint.
Nicki [00:01:18]:
And this has always been the discussion of kind of quiet the diet being somewhere in the middle of these two camps that we have. And I think that on one side we have people focusing solely on the physical component of hunger and appetite and cravings, and then on the other side we have a sole focus on the emotional aspect. And in reality, we can’t address one without the other because they’re both happening at the same time. So we have to be looking at both. And that’s what I’m excited to do today, is kind of break that down because that’s where we see the most impact is when we’re looking at both at the same time and kind of in that middle ground area.
Michelle [00:01:59]:
I’m concerned about that.
Nicki [00:02:00]:
I know. I was thinking the whole time, I was like, should I just stop?
Michelle [00:02:05]:
Yeah, we might have to redo that, but I think either one of us can do that. But it seems like it passed. I think we should yeah, I’ll just give it again. We don’t need to the whole episode again. But obviously whoever’s hearing, know, editing Phil or Kate, let’s cut out that part. Yeah, I hear coming back a little bit. I’m going to do this part. Mute your phone for a second just to let all of the ambulances pass.
Nicki [00:02:31]:
Oh, I think they’re good now.
Michelle [00:02:34]:
Okay.
Nicki [00:02:37]:
I’m really excited to talk about this middle area because I feel like we always talk about how quiet the diet is in that middle ground. And we have one camp that tends to focus solely on the physical component of hunger and appetite and cravings and then swing to the other end of the spectrum. Only some people are only focusing on the emotional side. And while both are very important and.
Michelle [00:03:04]:
What I hope to differentiate in this episode and what I think our podcast successfully differentiates, I mean, I don’t know if we’re successful in it, but we try to be successful in it is that we can work on any condition we have. Any appetite? Certainly not a condition, but any symptom we have from a physical standpoint or from an emotional standpoint. Appetite specifically is something that from a history vantage point, I think about appetite as being either it’s really scary that you have a big appetite or it’s really scary that you have a small appetite. If we think about our grandmothers would be like, oh my gosh, I’m so nervous. You’re not eating anything. Oh my gosh, what’s going on with your appetite? Because low appetite can certainly be a symptom of illness and having too much of an appetite is something that has been studied a lot because in ways of weight loss drugs, and in ways of what has historically been studied or pushed out from a drug perspective, really, appetite suppressants have been most impressive. So I guess the question that we’re going to be exploring today is also is a goal for weight loss to actually decrease our appetite? Is that something that is effective for weight loss? Is that something that’s safe for weight loss? And is the whole thing about weight loss really having this big genetic kind of appetite that people say, like, I tend to be more hungry than other people? Is that true? Let’s explore it. Let’s talk about the studies and let’s mostly talk about the mechanisms and the kind of understanding of what our body needs from a physical and mental standpoint.
Michelle [00:04:40]:
I’m so excited.
Nicki [00:04:40]:
I’m so excited. I think it’s really important too, because a lot of times we hear these words used interchangeably. So we hear people say, I have a big appetite or I’m really hungry, and in reality they’re a little bit different. So I think it could be useful to kind of define each of these terms before we kind of dive into using them for the next hour, please.
Michelle [00:05:02]:
Nicki, can you tell us what definition of hunger we’ve come up with?
Nicki [00:05:06]:
So hunger is basically that purely physical feeling of discomfort or weakness caused by a lack of food, empty stomach, coupled with the desire to eat just as a biological mechanism. Now, appetite is the desire to satisfy any bodily need, but in this case, we’re talking about food. So it’s more of that desire, whereas the hunger is that physical piece and then cravings would be a little bit more intense. So something like an urgent or sometimes abnormal desire or longing. Like where if you think about how you can’t stop thinking about that one.
Michelle [00:05:41]:
Thing and all three of these can be happening from, again, a physical or an emotional standpoint. It seems like you can have hunger without having an appetite. And we’ll talk about what that looks like. So it’s like you’re not driven to eat even though you are experiencing hunger. And there’s certainly some ways that our body will help us with that. If we don’t have access to food, we might naturally decrease our own appetite with the impending understanding that food isn’t coming. So that’s really important and interesting. I think a lot of what we’re going to talk about of those three terms is appetite today.
Michelle [00:06:17]:
I think that’s what we’re really going to be focused on, which is this desire to eat, and whether that desire is coming from a need or a want is what we’re going to explore for sure. And then cravings, we’re of course going to cover today too, because I think that’s going to be important for the listeners and something that really concerns people. And I know that cravings feel especially frightening for people because of that urgency piece of it. And also cravings can feel very irrational. So let’s talk about the physiology of hunger and appetite first. There are a couple of different pieces that go into and organ systems that go into how we experience hunger from a physical standpoint, or how we experience appetite from a physical standpoint. So the systems that we’re looking at is the brain, the gut, and our fat tissue. Those are the three ways that our body is going to signal and notify us that we should either get more food, get less food, and what types of foods we should be getting.
Michelle [00:07:14]:
Nicki, do you want to talk to us a little bit about the kind of brain gut connection when it comes to hunger and appetite specifically?
Nicki [00:07:22]:
So basically, we have these hormones, like you said, being released from different areas of the body, from our fat tissue, from our GI tract, from our brain. And so our hypothalamus, which is in our brain, is communicating with the GI tract through these hormones. So they’re like these messengers that are going back and forth. And so we have leptin is released from our fat tissue. And so leptin would be there to regulate our hunger levels and basically increase feelings of satiety or fullness. So the more fat tissue we have, the more leptin we’d be making. And then, hypothetically speaking, the more full we would feel. And so that’s leptin coming from our fat tissue and then regulating our hunger levels in that way.
Nicki [00:08:10]:
We also have ghrelin, which is produced by our stomach. So if you’re thinking about when your stomach is empty, we need to signal to our body that it’s time to eat. So ghrelin would be released by our stomach, small amounts by other areas of the body as well, and then it’s driving us to increase our appetite, take in more food, and also promote fat storage so that we can save that food for later, for energy.
Michelle [00:08:37]:
And thank you for our leptin and ghrelin talk when we were in our dietetics program, I remember them describing ghrelin like gremlin. So I would think like it’s like a little hunger gremlin that lets you know when you’re hungry. When we are talking about any of these things, we have to understand also that we can have a biological need to do something and then we can also react to that biological need. So there is always human input in these things. It’s not like if your leptin or ghrelin are dictating your decisions, but they’re going to push you. The reason these hormones in this system exist in the first place because our bodies are so brilliant that they really want us to keep a level of homeostasis when it comes to weight. They want us to keep balance and they want to keep us, I say this almost every episode, alive. Our bodies want to keep us alive.
Michelle [00:09:22]:
That is the primary goal of our bodies is to keep us alive. So if we have too much or too little fat tissue, that could become an issue. Now, what we’ve been seeing in the past, I would assume with highly processed foods, it could really be in the past 100 years, I guess a little bit less. But we’ve been seeing that there are certain foods that can influence these hormones over the homeostatic process. So this is a really important theory to understand, which is that our bodies want to keep us in this state of body fat. There’s a sweet spot for our body fat. It’s different for men and women. And if we are pushed out of that, what should happen is these hormones should be altered, especially leptin, to help us maintain a certain weight.
Michelle [00:10:09]:
So I find it very interesting when people say I am genetically predisposed to gain weight. There is definitely genetic basis for weight gain, but it matters a lot of what environment is placed on that genetic basis, right? We always say this is the thing you’ve heard on every Functional Medicine podcast. Every listener has heard that genetics loads the gun and the environment pulls the trigger, right? So the thing that pulls the trigger for these hormones to be altered is really two things, these hyper processed foods and the end result of those being inflammation. So what can happen with these hormones that are meant to keep us at a certain body fat level, a certain weight, is that they can become altered so that the signals start getting wonky. And that happens with rapid weight loss. That happens with weight gain. That happens with the consumption of these foods. Overall, inflammation, even environmental toxins can cause and influence this.
Michelle [00:11:01]:
So what happens is that you might have the right amount of, let’s say this leptin hormone, which again, when you lose weight, leptin adapts, it drops to meet the body fat or weight level that you’re at. What ends up happening is when leptin goes low, the body goes, oh my gosh, now I need to increase food, need to make sure that this person’s staying in homeostasis and I’m going to slow down my metabolic process. So again, anytime that our body goes in either direction, ideally what would happen is we would actually gain weight and then when we gain weight, our appetite would actually decrease. That would be the goal because then our body would say, hey, we’ve had enough. But what happens is there’s certain chemicals in food that can end inflammation itself that can push and make these leptin receptors resistant, which means that the more weight you gain, actually the more weight you would continue to gain. And we know like Prater willie syndrome, which is we now recognize as a leptin disorder, is when people have like an insatiable appetite no matter what. And I think about, again, with leptin, it’s not only the total amount that you have, but it matters if your body is recognizing that you have it. So leptin is just a really important hormone to understand.
Michelle [00:12:18]:
It’s really important to understand that it doesn’t really matter if you’re at the right weight. Your set point, that weight that your body thinks you can be at, can continue to increase if we continue to be inflamed and if we continue to blunt those signals. Did I miss anything in that theory? Nicki, anything you want to add?
Nicki [00:12:34]:
No, I’m glad that you brought up the leptin resistance piece because there can be, as we said, it is a direct correlation with the amount of fat mass that your body has. But we could have two people with the same fat mass and different reactions or responses to leptin because 1 may be leptin resistant and the other would be more sensitive to it.
Michelle [00:12:53]:
Absolutely. And from a weight loss perspective, I know this focus is really on appetite and there’s a direct correlation between leptin and appetite. There’s a direct correlation between ghrelin and appetite. But when it comes to weight loss, something I’ve spoken about on other podcasts before is this Biggest Loser study that was done, which was that they followed 15 contestants from The Biggest Losers came out in 2016. And of the 15, a majority of them, I believe it was 14 out of 15, either gained all of the weight that they had lost or they had not kept off. At least 50% of it was like 50% or more they had regained. And I guess the initial thought that people had was that they kind of got home from the ranch and started eating like crazy, stopped working out and that really wasn’t the case at all. What happened was their metabolisms had adjusted so drastically that their body was driven to the state of a slow metabolism and their metabolic rate had decreased rapidly and at the same time a much higher increased appetite.
Michelle [00:13:53]:
So they weren’t all acting on that appetite by the way. They weren’t acting on that hunger, but they still were regaining the weight. So it was very upsetting study, by the way, but it let us know a little bit more about this leptin and leptin resistance piece and how that influences appetite and hunger. So it’s just really important to understand again, that by the way, there’s a diet called the Leptin diet. And the Leptin diet really focuses on eating very bland foods. So that you’re not combining things in this very hyper, palatable, high dopamine kind of way that can really help. It’s purported to help with leptin levels and also can help with appetite and hunger. So I know that we spent a nice chunk of this time talking about leptin, but it’s one really important way that our body regulates appetite.
Michelle [00:14:40]:
And for you to understand that if you are in a larger body and you’re like, why is my body not stopping getting larger? Why is my body continuing to want those things? It’s because your body might not be recognizing that hormonal signal. So I know that was a lot bite off and thank you Nicki, for walking us through it too.
Nicki [00:14:57]:
And so, as important as leptin and ghrelin are in terms of hunger hormones, there are other neurotransmitters, other hormones in our body. From a physical standpoint, we’re definitely going to get into the emotional and the social standpoint. But from a physical standpoint, there are other things that also can affect our appetite. One being, I think this is a very commonly discussed topic, I believe, when it comes to serotonin. So, as you were saying, with processed foods, specifically refined sugars, refined carbohydrates, our body starts to learn this response of consuming carbohydrates, particularly refined and processed carbs, and then it causes our body to release more serotonin, which is our happy hormone. So if we are feeling sad, upset, depressed, whatever we’re feeling, we start to now seek out these foods to increase our serotonin levels and feel better. And so that’s when we start to have increased cravings and appetite for those foods in particular. And serotonin also reduces pain and regulates our mood.
Nicki [00:16:05]:
So even if we’re in physical or emotional pain, we have that physiological response to seek out these highly palatable, highly processed foods to make ourselves feel better.
Michelle [00:16:17]:
Yeah, this is a really important piece that again, we’re pulling together, which is that we have, again, these basic biological needs to stay alive, biological need to maintain homeostasis. But when these newer foods were introduced to our bodies, they kind of were better than homeostasis. Our bodies were like, wait, if we can be balanced or we can be amazing and we can feel really good. So it’s super normal to also want or crave these foods more. And it’s also a challenge that’s been unique to us in the past 100 years, I believe, because whereby in the past you might have gained weight from eating whatever, like more whole, real foods, now the weight gain is accompanied by this hormonal change, which also then leads to more weight gain and puts us in this pretty tough cycle. And I think just having this I keep hammering it in, but having this one baseline understanding that our bodies do not want to gain weight, but that things can influence us to want us to gain weight and to override that homeostatic process is really important to understand. Thank you for adding that too, Nicki. That’s super important.
Michelle [00:17:29]:
And then when it comes to hormones, again, we’re talking about this physical piece or the hormonal piece. Of course, things like insulin can, like you said, because of those carbohydrates, insulin can influence our appetite as well. So can cortisol. And let’s talk a little bit more about cortisol specifically. Nicki, and how that influences our appetite.
Nicki [00:17:48]:
Yeah, so cortisol also is our stress hormone. When we are stressed, as I kind of said before, a little bit about the serotonin piece, our body so acutely, which in the short term high cortisol or high stress actually suppresses our appetite. So that’s in a situation where you might find something kind of hits you really hard that day and all of a sudden you realize it’s been hours and you haven’t eaten anything. So that’s that acute level of stress. Now when that is present chronically, which is unfortunately most of our lives, especially in New York City, we are noticing that cortisol increases our appetite over time for specifically those hyperpalatable, really high fat, calorie dense foods and it also activates that reward center in our brain. Now what was interesting was they did a study, there was a study published in the journal Addiction in 2022 that showed that this response actually becomes, it perpetuates itself over time. So first we have a response to seek out these hyperpalatable foods when our cortisol is chronically elevated. But now the more we engage in that behavior, the less satisfaction we actually get from that food.
Nicki [00:19:08]:
And so then we actually need to eat more to get the same response. So this is now a programmed response and cycle that’s happening. But of course, like anything else, it can be deprogrammed. It’s just a matter of kind of pulling back from those foods and creating a different kind of like breaking that cycle which we’ll talk about. But if you find yourself in that cycle, it has a physiological basis.
Michelle [00:19:34]:
Yes. And I think what is going to set this podcast hold on, what is going to set this podcast apart from other podcasts on the topic is again, we are applying immense compassion when we talk about these topics. So we understand completely that what we’re kind of up against are these superhuman foods that are creating a new need for appetite and hunger. And that appetite or hunger is very real. So I want people to understand that if you are feeling those cravings, I believe you 100%. And I also want to say I really don’t believe it’s your fault. And I have so much empathy for that. And I also want you to not feel scared because there’s so much we can do.
Michelle [00:20:16]:
So it’s not scary and I want people to not if you’re feeling, again a little overwhelmed by this information, take a nice deep breath and just know that this is a solution based conversation. We’re not saying oh my god, these big bad scary foods or anything like that. And we’ll talk about how it can be risky to do that too, but that there is something going on here. It’s not just that people are very gluttonous by trade or something like terrible and judgmental, but truly there is something spectacular about these foods that causes really strong physical changes in people. And I think what immediately from a quiet the diet perspective jumps out to me is if someone liberalized kind of all of these food restrictions, would adding these foods in eliminate all of their cravings? And the answer from this study is no, you would still have an increased need and increased cravings. And by the way, one very interesting thing we didn’t talk about, that we both learned in our dietetics degree is that food companies are aware of these responses, so aware that they can measure these responses. And I’m so upset that I don’t have the exact study, but there are studies that food companies have done where they will literally attach electrodes to people’s brains and actually measure brain activity around different foods. So much so they can determine how often someone is going to come back for the same food based on how much it lights up the brain.
Michelle [00:21:50]:
And from a cortisol perspective, the reason why our bodies in acute stress don’t want food. And some people, by the way, during those stressful times do reach for food and it is comforting to them. But when we’re having something like a panic attack, we might feel a little more nauseous, we might have a decrease in appetite is because our body is diverting all of its blood supply and resources to other parts of the body so we can fight flight or freeze. So our body is like it’s not time to eat. We’re trying to survive here in a longer term way. Cortisol is also much like insulin, a fat storage hormone. It is a hormone of preservation and survival. So our bodies don’t understand the difference between starvation and high stress.
Michelle [00:22:28]:
So our bodies are going to want to hold on to food in case a famine is coming. And we crave these very dense foods in fat, sugar, salt and carbs specifically because those foods are going to last us the longest in that famine. So our bodies have been designed, again our beautiful brilliant bodies to save our lives and all for preservation. And we’re now in a place where food diversity is so abundant in ways of kind of food and what I would call those food like commodities, those hyper palatable foods for many of us and not for all of us. And that’s really important to acknowledge too, because we’re going to talk about that also that our brains, I don’t feel, have and this is subjective just a feeling. I don’t feel our brains have adjusted to the wonders of all of these foods in any way. They still are as stimulating as they have been and in fact, our need continues to increase for these foods.
Nicki [00:23:21]:
Well, it’s interesting that that just reminded me of this other piece that we had in our little outline to talk about little it’s like because I think some people have noticed this correlation in their own bodies when they have a lack of sleep that they have an increased drive for certain foods. But what was interesting was the study that we found that showed that this drive actually acting upon the drive was solely dependent on the availability of that food. So at least in the setting of lack of sleep because that’s what this study was looking at when we are more sleep deprived and it’s also directly correlated proportionally. So the more sleep you lose, the more appetite you have for these highly palatable foods. Now, when they put these two groups in a setting where they had availability to food and where they didn’t.
Michelle [00:24:24]:
The.
Nicki [00:24:25]:
People who were in a setting with a wide variety of foods consumed more of them. And so if we’re taking that out of context, out of context of the study and kind of putting it in context of our real lives, the availability of these foods and the access that we have to them is part of the puzzle. So again, as Michelle was saying, not sometimes we can feel like oh, I just don’t have willpower. I’m not disciplined enough. We are at odds with this multi billion dollar industry that’s shoving these advertisements in our face. We’re constantly surrounded by certain foods. And so that’s when we also have to notice that it isn’t just your willpower. There are other pieces at play, whether it’s that social piece or this physiological aspect.
Michelle [00:25:18]:
And let’s just in ways of food availability, accessibility and what we have in front of us. What kind of would verify this on a more epidemiological level is if we think about food deserts or food insecure neighborhoods of people, the likelihood of disease and weight gain or being in. I’m going to put in quotes the category of obese because we know it’s a term that can be triggering for people. When we think about that, the likelihood of being in those neighborhoods and having food insecurity and still the only food you actually have available to you is the hyper processed foods. The question that we always ask is like how do people have low access to foods gain weight? And it’s because the likelihood that you’re going to be attacked and hunted by these food companies is even higher in those neighborhoods. And the access to fresh meat, fresh fruits and vegetables actually goes down. That’s what actually would make it a food desert is actually access to more of those foods versus access to just the hyper palatable foods. So I think that it’s disproportionately gross.
Michelle [00:26:23]:
I don’t know the word like horrible and also lets us know that, again, weight gain is less no matter what financial situation people are in, and of course marginalized people are going to be in a harder decision making position and in a harder marketing position. Unfortunately, they’re going to be marketed to harder. It lets us understand more of why those foods are an even bigger concern, which is really frustrating.
Nicki [00:26:53]:
I know you were looking for the word. It’s like predatory is what it is.
Michelle [00:26:56]:
It’s totally predatory. I know I’m being gentle because it’s a podcast episode, but it’s like grotesque and that’s the truth. And why people don’t have always asked or not understood why people who people encounter more chronic illness or encounter more weight issues or are obese in those conditions. And it’s because of even you can have a deep nutrient need and a deep physiological need and these foods will give you the most bang for your buck in ways of calories and nutrients, but they create an entire storm of appetite and weight gain issues. So again, a little depressing. I know, I understand reality is not what I expected when I was a kid, but certainly something to acknowledge and certainly, if anything, should give even more empathy and less judgment to people who have lower access to foods. But again, like you said, Nicki, what’s in front of you and what’s available to you is what you’re going to eat. For many of us, the only thing available to us are these hyper palatable foods and these highly processed foods.
Michelle [00:28:02]:
So the accessibility to processed foods is at an all time high and our ability to buy it is at an all time high. So it’s also going to create an environment where it’s extremely hard to kind of fight against what we’re seeing from an appetite perspective.
Nicki [00:28:20]:
But as we know, as we mentioned earlier, when we start to break that cycle and choose when available to us, more unprocessed, more whole foods, we start to then crave those hyper palatable foods less because they have more of an impact on us. So there is some of this power that we can take back when we have access and when we have availability to break into that cycle and kind of shift our appetite. It’s kind of like in a combination of all of these hormones and neurotransmitters. It’s working on that physiological level to then affect our appetite in a positive way, in a way that we seek out foods that are more nutrient rich. And so you’re not kind of I know it feels like you’re stuck in this cycle and that it’s hard to kind of see a way. Out when you’re in the middle of it. But just know it’s just that putting 1ft in front of the other and just making each time you have the option to make this choice, you’re slowly just stepping one step at a time outside of that cycle.
Michelle [00:29:27]:
Oh yeah, I think we have 100% of the power. I think we are the powers that be. I don’t think the system is the powers that be. I think we are the powers that be. Honestly, and I agree with you completely and I appreciate you saying that too. It’s interesting because I feel if I were to kind of classify where we’re at as a nation right now, I’d say we’re over calorie and very undernourished. I think we are very lacking in nutrients and very overstressed, which makes you deplete nutrients quicker. And I feel that we have too many it’s not calories, but it’s too much food to nutrient ratio.
Michelle [00:30:02]:
Essentially too much calorie bang for your buck compared to nutrients. So it’s interesting when people talk to us about cravings from this physical standpoint, if we kind of switch the conversation to cravings a little bit, I think people feel really compelled to think that cravings come from specific food needs. And it’s really interesting because we now know that foods themselves can cause cravings. But there are some instances, Nicki, where food cravings are actually from this deep biological need. But I think people know before they start a somatic or an intuitive eating journey, they’re trying to understand what does my body need from a nutritional standpoint. And there’s so many things that can make that signal wonky. It’s not always reliable. Sometimes we have to take action first and we just have to say, hey, I’m not going to eat hyperprocessed foods for a little bit, or whatever it is.
Michelle [00:30:53]:
And then the body signals can come back online. But because those foods change our physiological signals, we can’t actually understand our cravings. I do want to talk about cravings from a very physiological sense first, before we talk about the hijacking of foods. As an example, let’s go through pika is really interesting and always been interesting as a dietitian. You learned in school a lot. Let’s talk about Pika.
Nicki [00:31:18]:
So Pika is if you haven’t heard of Pika, it’s a craving for a non nutritive substance. It just means like a non food craving. Now it’s typically seen in iron deficiency anemia, also instances in pregnancy, also instances of low zinc or calcium. And we know that supplementation with these nutrients stops the behavior. And so this might come in the form of like a craving. I think they actually had a show on MTV at one point.
Michelle [00:31:47]:
That my strange addiction. I was just thinking about that. I literally was thinking about it. I’m like the people who I just saw an episode of that recently. I think it’s on one of the streaming channels now. And the man was addicted to tuna fish and he would like wipe it on his face. And it was very funny and very interesting, but also felt very bad. But yes, my strange addiction is people consuming non food products.
Michelle [00:32:07]:
I wonder if we ran a nutrient panel on them, what would come up?
Nicki [00:32:10]:
Yeah, and I know that there was an episode and it’s exactly like listed in pika, ice, dirt, soil, like laundry, just stuff that it’s like there’s kids that eat the wall, just stuff that they need to chew on. And so in that instance yes, that behavior is caused directly by a nutrient deficiency. There’s still question as to why exactly that’s happening, like what the actual mechanism is for that. But that is one example of a very clear distinction between deficiency and craving.
Michelle [00:32:46]:
Yeah. So it causes craving very much and the fact that it is resolved through that makes it very physiological. It’s really interesting because the specific deficiency you’re talking about is iron. Another deficiency, another mineral deficiency specifically that is fascinating is salt. So tell us about the American Journal of Clinical Nutrition study. It was from 1990, but it’s still interesting. Tell us about that, Nicki. You’re a study.
Nicki [00:33:13]:
I mean, we love salt. It’s season three. I feel like everyone knows we love salt.
Michelle [00:33:17]:
Come on. We had Amanda Montalvo in episode two, of course.
Nicki [00:33:21]:
So in this study they fed patients a very low sodium diet but also gave them diuretics to really deplete their sodium levels. In this instance they did have an increased preference for high salt foods. So that was a very clear distinction between low salt intake driving a craving for more salt. Now conversely, we also see that on the opposite end of the spectrum. So the more salt we eat, if we’re maybe consuming more takeout restaurant food, more fast food where we have a very high proportion of sodium in our diet, that also can increase our preference over time. So now you might notice, oh, I crave salt a lot. Now it can be from one or the other. Maybe it can be consuming a lot of salt or consuming not enough salt.
Nicki [00:34:13]:
But it was interesting that that was one mineral that we saw. Another direct correlation, which leads me to.
Michelle [00:34:20]:
My hypothesis of the day, which is that maybe what our body is best at communicating with us is mineral cravings, which is the most essential component of life. How good is our body at communicating something like carbohydrate cravings? Is that the same thing? And also we have a little bit of knowledge of this because if we get low blood sugar, we actually can get a carb craving. Our sponsor for today’s episode is very you’ll have heard about them a little bit before. But it’s really interesting Nicki, because when my blood sugar is high, I might notice sugar cravings. When my blood sugar is low I get really cortisol y. So I actually stop feeling hungry. So it’s interesting because I don’t always trust necessarily a sugar craving could be either for me. It’s really interesting.
Michelle [00:35:15]:
And like you’re saying about salt, I definitely experienced that for myself, which is why I’ve gotten so much information from continuous glucose monitors. Like very specifically, very because I get that body feedback to understand and then I can read those signals a little bit clearer. Now, I think listening to your body is paramount, but sometimes to just weed out those signals, it’s really powerful to have a tool like that. So tell us a little bit more about carbohydrates and kind of let’s move on from minerals and talk more about cravings. When it comes to carbs and protein and fat.
Nicki [00:35:44]:
Yeah, by the way, I also have that if my blood sugar is too high or too low, I also am craving carbs. So it is a very interesting, just like anecdotal experience. But now when it comes to macronutrient, having a low intake of certain macronutrients, and that driving cravings, the studies are a little bit more inconclusive. But there was a study in the journal Appetite from 2006 that showed that they restricted carbohydrates, but actually complex carbohydrates. So fiber filled carbs, not just refined.
Michelle [00:36:16]:
Carbs, the ones that most nutritionists would recommend, like those kind of foods.
Nicki [00:36:20]:
And as they restricted those for three days, there was an increased craving. They saw increased carbohydrate cravings and consumption in that period where they were allowed to eat whatever they wanted afterward. And we know our body runs on glucose. Our body needs carbohydrates to function. So that makes complete sense that we don’t have enough for three days and we’re going to have an increased drive and increased consumption afterward.
Michelle [00:36:48]:
However, and we’re aware of this, our body at some point might defer to other fuel sources like ketones. Which is why when you hear about ketosis and things like that so people who are operating from a place of ketosis, where ketones are their fuel source primarily. Actually, I have seen many studies that substantiate that. People in ketosis do have lower sugar cravings over time, but there are hormones that are reliant on those carbohydrates for production. Like our thyroid hormones require a certain amount of carbohydrates for production. The craving gets blunted so much that we might not know that we need those carbohydrates.
Nicki [00:37:31]:
And this study only restricted for three days. So it can be a situation where we know that it does take a little bit of time to get into ketosis. So I’m curious, like you guys mentioned, if they dragged us out a little bit longer, if that would have shifted the impact afterwards, it’s really hard to.
Michelle [00:37:48]:
Just rely on our I don’t like what I’m about to say, but it’s true is that it’s so hard to rely on just our body signals to understand everything that’s going on. Because also when you restrict carbohydrates in the beginning, you actually can get a surge of energy and then a really quick drop off or it could be hurting you on the back end by altering your sleep, your anxiety, your stress hormones, things like that. And you might not notice it for some time. So I think experimentation is really important with diet and to notice how you feel. But sometimes how you feel is not the whole picture. Sometimes it’s just important to know like if I have hypothyroidism, I need to have X amount of carbohydrates in a day because that’s how much it takes for my thyroid to function. Usually like 130 at least, which is a lot more than ketosis. So I think that’s the complicated part of the macronutrient piece of the puzzle, which I think is one of those missing pieces of intuitive eating too, which is that if you liberalize all food restrictions and you eat in a way that you access your hunger cues.
Michelle [00:38:49]:
I don’t believe our hunger cues always tell us the full picture of what might be going on. And you might have some sort of deficiency and let’s say you had a vitamin B Twelve deficiency or something like that. You might feel really anxious and have numbness and dizziness and things like that. But that doesn’t translate into I need to go have a piece of meat. In fact, vitamin B Twelve is really interesting because there’s a high correlation between where absorption happens primarily in the stomach between B Twelve production and acid reflux. Now, I’m going to talk about acid reflux specifically as we go into our second macronutrient when it comes to cravings, which is protein. Protein is one of the most complicated nutrients when it comes to cravings because it is the most satiating macronutrient, which means that we feel the most satisfied when eating protein. From a hormone perspective, like we were talking about from ghrelin and leptin, from that kind of more ghrelin and CKK and other gut hormones.
Michelle [00:39:54]:
CCK and other gut hormones. But protein, when we have a protein deficiency and we can look at Dr. Gabrielle Lyon’s work for what the real definition of protein deficiency is, we do not always have an increased craving for protein. So I notice so often that my clients are grossly undereating protein and the equation I use for protein is 1 gram per pound of ideal body weight also from Dr. Gabrielle Lyon and do not want protein, they do not want to eat animal meat. And what happens is our body when we have lower stomach acid which can happen over not consuming enough protein over time, not having good bile flow, a bunch of different reasons, any kind of again toxic and anything like that, we actually crave less protein. And this is our body’s way of again, yes, you can imagine it saving our lives, right? We don’t want to introduce a lot of protein in a place where we can’t break it down so our body stops craving it as much. So there are some things you just kind of have to do with your health that you know are right and then feel the benefits later on because in the short term you might not feel good listening to those cravings or things like that.
Michelle [00:41:04]:
Like if you’re on a long term vegan diet, you are going to stop craving protein, most likely, but it doesn’t mean you don’t need it. You need it more. It’s just that your body doesn’t think that it can incorporate it.
Nicki [00:41:14]:
And that’s why those are the only studies that we really had in this section of the podcast because there’s just not conclusive. So, like what you said about really what quiet the diet is all about is pairing. Yes, listening to our body, figuring out what our body needs, but also pairing that with this concrete nutritional science information because we really do need the two, especially in this modern world that we live in, we really do need to pair the two together to have optimal health and optimal body organ function.
Michelle [00:41:47]:
So half the time we have to do the stuff that we know is good for us. I love that there was like this instagram trend where people were like, I’m going to drink my stupid water and go on my stupid walk. And I thought that was the cutest thing because sometimes we just have to do the things that we know are important for us and find a way to make them palatable and do. And then sometimes we can just rely on our body cues. This is the beauty of all of this. The more that we do the things that are awesome for us and we correct what’s going on underneath, the more clear our body cues become and we can listen more clearly. By the time clients come to work with either of us, Nicki, they usually don’t have clear conversation between their body and brain. It’s the same way where if someone has like a histamine intolerance, that can cause panic attacks and it’s because we’re not understanding what is that symptom showing us.
Michelle [00:42:35]:
And I think that when it comes to cravings and appetite, we get mixed signals because of this complex hormonal cascade, because of all of these different areas where we’re getting information. And so sometimes we just have to do stuff and then also feel at the same time. And sometimes we just feel. So let’s talk also about okay, let’s talk about drugs for a second. Let’s talk about drugs. Nicki. Let’s talk about drugs for a know it’s been again, from the kind of physical weight loss camp and the physical appetite suppression camp came a lot of these drugs that really focus on just that, appetite suppression. We’ve never done a mention of it.
Michelle [00:43:20]:
Let’s do a little mention of the GLP One inhibitors, ozempic Manjaro, Wegovy, the drugs that you all heard of before. Why were these unique or interesting from an appetite perspective?
Nicki [00:43:33]:
So GLP One inhibitors are very interesting because they are interacting in many different ways to increase our levels of satiety. So, so many of the components that we talked about earlier in this episode, they’re acting on. So they’re interacting with ghrelin and leptin, our hunger and fullness hormones, they’re interacting with that reward center in our brain. They’re also influencing the beta cells in our pancreas, which are the cells that produce insulin. And then from a completely physical mechanical standpoint, they’re also slowing down the rate that our stomach is emptying and so we’re fuller for longer, in which case our appetite is also decreased. So we’re noticing that these drugs are directly impacting these hormones and these processes in the body. And the focus is that I don’t know how to say this without like trying. I don’t want to shame anyone.
Nicki [00:44:42]:
I was going to say we become reliant on them and then when we stop, you know what I mean?
Michelle [00:44:49]:
Yes. So I would say that. All right, I’ll do this part.
Nicki [00:44:53]:
Yeah.
Michelle [00:44:54]:
I think what was unique about these drugs is that they created a very specific and noticeable decrease in not only people’s appetite, but the diet chatter that people felt, oh, I want this food. I want this food and those cravings and everything like that, that seems to be wildly successful for some people and not as successful for other people. What I think of course, the concern always is, Nicki, when you go off of these drugs, does that support end? Do you need to continue the drugs or is it making legitimate hormone alterations that are permanent to help with appetite?
Nicki [00:45:34]:
So that’s the real problem is that we’re noticing A, people are losing weight pretty rapidly and we know, as you had mentioned, the Biggest Loser study, when we’re losing weight. So let’s say someone used to be in a larger body and then they lose weight and now they’re at the same body size as someone else who’s always been that body size. Their levels of leptin and ghrelin are different, so they never go back to where they should be in someone who has always been that body size. So now we’re kind of faced with this double whammy where now our appetite is increased, we’re at this lower body weight, but we have more of a drive for food. We’re thinking about food more and now we don’t have that external support from the drug. And so it can be very difficult to maintain that weight loss over time because of those drivers that are really pushing us to reach for food.
Michelle [00:46:31]:
Absolutely. I think, again, if this is a completely individual decision that people make, and for some people it might be worth it to have the drugs in the short term and get the weight loss and then deal with the after effects. After or if there’s no after effects, we can’t say what it is for every single person. I think what’s so interesting and what I was obsessed with learning in school was that what makes weight loss surgery so successful is not and so successful meaning the rates of weight lost and kept off are much higher than through any other diet. Means is actually because weight loss surgery alters those hormones that we’re talking about that influence appetite and cravings, that influence our body’s understanding of what weight or set point we should be. So this was something that I always thought it was like, oh, they just forces them to eat less because they can’t fit anything. People can’t fit anything in their gut. And that is part of it, by the way, too.
Michelle [00:47:32]:
But it’s also because when our gut is full, it will influence how much that gremlin ghrelin is fired off. If our stomach is empty, then we experience more ghrelin. If it takes less to fill up your stomach, the ghrelin is released and as you gain more weight and again you have more fat or more body fat percentage per pound, those levels are going to be altered or that leptin can become resistant and you will not be able to feel satisfied. So weight loss surgery has kind of did the opposite. Now, I have to say, I have people who’ve been very successful clients, who’ve been very successful weight loss surgery, clients who felt like it, for lack of a better term, ruined their entire lives. Some people, it saved their lives. Every single thing we’re talking about. There’s not one recommendation in this show for what anyone should do for themselves, but it is to say that there is some real biochemical things going on with appetite that extends beyond just our relationship with food.
Michelle [00:48:30]:
But we do think our relationship with food is important too. So we’re going to talk about that. So we’ve kind of talked about for 50 minutes the physical components of appetite and hunger and how appetite and hunger can be influenced. Again, from this hormonal standpoint, this brain standpoint, gut standpoint, everything like that. Let’s start and open up this conversation from the psychological standpoint. Now, again, current culture would tell us that cravings come from restriction. The more food you restrict, the more you crave food. There’s certainly a science to support that.
Michelle [00:49:02]:
Nicki, tell us about that.
Nicki [00:49:04]:
Yeah, so this is incredibly interesting because of course we know that when we’re physically restricting foods, we crave more foods. Now, evolutionarily, we need that process because our body needs food to survive. So that makes complete sense. Now, we hear a lot from clients saying, I’m not restricting, I’m eating foods and I’m still craving as if I was physically restricting. I don’t know why this is happening. So we know that in the research we can see that that psychological restriction can actually have a very similar response as the physical restriction. So what we mean by psychological restriction is even if we’re eating the same amount of foods we are either maybe we’re feeling a little bit of guilt or shame around the food or we’re saying I’ll never have that again, or I’m not going to have that, I’m just going to have a bite. And maybe at the end of the day we’re eating the same, maybe even more than we were before.
Nicki [00:50:10]:
But those cravings are still there because in our mind we still have this scarcity mindset as if we’re not going to see that food again. And if we’re thinking about our ancestors, if we were never going to see a food again, we have to get it all in now because it’s not going to be there tomorrow.
Michelle [00:50:28]:
This is so fascinating when it comes to elimination diets and other kind of matters of chronic illness therapeutic interventions for diet. Because I’ll have clients who are eating a lot of food for them but they are adopting when they come to me like a paleo diet or something like that. And they feel like they are so restricted and angry about it that they end up just eating like handfuls of nuts because their mental feeling is that they’re being very restricted. So I think when we get into a dangerous zone is when we start restricting foods that are whole real foods. That’s where I think especially that restriction piece comes in handy. And I would be interested to see future studies that show like if we restrict, quote unquote, hyper palatable foods, but we eat a variety of any food that is real food or something like that, it would have the same effect. But regardless of that, I think there would be some sort of feeling of you can’t have that. Okay, I’m going to starve, let me get more of it.
Michelle [00:51:33]:
So the point is that the language you use around food and how much we restrict ourselves is extremely important for appetite. And this is really important also when we talk about that kind of victim mentality and feeling like this is unfair, this is only happening to me. I’m in the state of chronic illness, which we’ve talked about in a lot of other episodes too. It’s just really important to be selective with how you are talking around those foods. I, for instance, I don’t feel any sort of restriction around food. I just don’t choose to eat foods that don’t make me feel awesome. So I just know that for myself, I am at this point where now, again, the kind of signals are clear for me and I can understand what I’m craving or I don’t really have cravings, but what I’m interested. In or have an appetite for specifically because I’ve done really hard mental work to make sure that I know I feel safe eating those foods if I want to.
Michelle [00:52:28]:
But it’s a difference between kind of phrasing things with I choose to eat these foods or I can’t eat these food. But really just emphasizing that study, Nicki, which is that even the mental restriction can feel like a physical restriction and drive our appetite up even more. And then if our appetite’s high but we’re not eating, that’s when we get grumpy and hangry, I’m sure, even if we’re not actually hungry.
Nicki [00:52:51]:
And I think one of the most interesting things was the thoughts around weight. So when we focus so much on restriction from a weight focus perspective, so trying to reduce our weight, you might be one of those people, you might know one of these people that every day kind of revolves around my pursuit of weight loss. Now, cravings were actually higher in women who were more frequently concerned about their weight, even if they were eating the same amount. So as you said, Michelle, if we shift that focus away from that urgency about weight loss, if we’re shifting that into, okay, let me take a step back, maybe give myself a month or two to really just focus on what are my body sensations, how do foods actually make me feel? And we’re pulling a little bit away from the weight focus and more onto that internal focus on how our body feels. We might notice that cravings actually reduce because that feeling of psychological restriction is actually decreasing, which then at the end of the day will actually make weight loss easier because you are craving less foods and your appetite is lower from.
Michelle [00:54:04]:
This very high level silly standpoint. I always say weight loss is the kind of thing you kind of have to side eye. Because if you look directly at it and you say, I’m going to lose weight, I’m going to lose weight, even if it doesn’t make you not lose weight from a physical standpoint, which can be argued, it’s definitely going to make your cravings worse and make the entire journey much more torturous. If you’re trying to lose weight. So I think that unless you are someone who is also grossly undereating, in which case our body is going to slow down our metabolism and potentially cravings in order to accommodate for that, which is that phrase we hear all the time, the starvation mode kind of phrase. What would you say about even the condition of anorexia nervosa? Nicki, I know you’ve done work in eating disorder facilities as well. Can you tell us a little bit about the adaptation of appetite when it comes to long term eating disorders?
Nicki [00:55:00]:
So it’s interesting because in and I’m sure you’ve heard about the Minnesota Starvation study, this is really telling us that when we are physically restricting, when we are grossly undereating, we have a increased drive for food even if we’re not acting upon it. So in a case like anorexia nervosa, we’re not acting upon it, but we are thinking about food all day long. So one of the indicators for how severe an eating disorder is is also, of course, all of the physical measures, but also asking clients, what percentage of the day are you actually thinking about food, because we notice that when that percentage is high, there’s some level of restriction there. And usually the higher it is, the higher the restriction is. So overall, even though we might start to think, oh, maybe their appetite is lower and that’s why they’re not eating as much. Appetite actually is driven way up because our body is desperately searching for food.
Michelle [00:56:04]:
It’s interesting because again, this word appetite now comes down to it’s not necessarily even appetite being manifested as I want this particular food, but it turns into just an obsession over food instead. So it’s not that the appetite is showing up as thoughts, that’s how the appetite is showing up because it has no other place to go because people aren’t eating in that situation. So I’m assuming that someone who was starving from a non elective situation so something that was not anorexia nervosa but just starvation, they would also because of low food I’m assuming the situation would be low food access. They would also have those very intense thoughts around food as well, long after we found in this study that a lot of people reference, a lot of the time, even that would drive again that biological need to eat food. And it would be manifested in eating a lot, I’m assuming, after, which is when we get into that realm of Refeeding syndrome and concerns around that and also that mental obsession with food. So either physical or mental restriction of food can lead to obsessive thoughts about food and or an increased appetite.
Nicki [00:57:20]:
And I know that when we’re talking about those studies and when we’re talking about eating disorders, we’re talking about a long term period of restriction. We also see this every day in clients who we’re skipping breakfast, we’re having a smaller lunch, and then all of a sudden I don’t know what’s happening, I’m having these cravings at three or 04:00 p.m. And they’re uncontrollable. And then we start to really spread that intake out over the day. Really get those nutrients in in the morning, focus on those in the afternoon, maybe having an afternoon snack and also doing that work to alleviate some of the shame around it. Reminding ourselves, my body needs this. I’m nourishing myself. These are nutrient dense foods that all of a sudden, we notice.
Nicki [00:58:02]:
Most of the time, those thoughts and daydreams about food in the mid afternoon start to really go away.
Michelle [00:58:10]:
Absolutely. Because hunger can cause appetite again just as much as mental restriction can. And for those reasons, intermittent fasting can be very functional for people’s appetite, in that I actually notice people have a lot less food noise if they are doing intermittent fasting for a while. The long term consequences on our hormones might then lead to alterations in these hunger hormones. In the long term, if the body is mimicking a state of starvation for a long time, which is again because our body is going to be desperate. Then eventually to get our weight up. And now the more kind of conversation I’ve seen around intermittent fasting, the less excited I am about it, to be honest with you. Because certainly in the beginning I think when we were implementing intermittent fasting, it was like that 16, eight, but then taking some breaks sometimes now people are going even more militant, only eating 1 hour a day.
Michelle [00:59:03]:
And I think that certainly I notice the alterations in people’s hormones, especially women’s hormones, especially menstruating women’s hormones, and how detrimental it can be on those exact hormones that cause hunger in the long term. So while you might have your hunger kicked for a little bit because your blood sugar is lower and you’re not having those fluctuations and your body is allowed to enables autophagy and all of those positive things in the long term, I still question the influence on our hunger hormones and everything like that because it influences insulin, cortisol and all of those things. For some people, positively, and for some people, negatively. So all of this is to say that if you are feeling ravenous hunger or you’re feeling like your appetite is too high and that’s what’s holding you back from weight loss or it just scares you. First of all, it’s not scary. It’s okay. We don’t want you to feel scared by this conversation at all. We want you to feel soothed.
Michelle [00:59:58]:
We just first want to say that it could be coming from a nutrient, a literally mineral deficiency perspective could be one of the reasons it could be coming from a macronutrient perspective. But the studies aren’t as solid on that. I think carbs are maybe one of the macronutrients that we do tend to crave a little bit more when we need it more. And certainly sugar, specifically when our blood sugar is low. And also can be coming from a mental restriction perspective. That’s what could be making your appetite very high. Consistent intake of hyper palatable, hyperprocessed foods also can make your appetite higher and your body’s metabolic capacity lower because it can influence your body’s ability to recognize leptin and that it has enough leptin. So I guess in extreme brevity for my tip to leave with is that sometimes our cravings are real in that they are indicating that we should get a nutrient in, and sometimes they are coming from stress, sometimes they are coming from hormonal imbalances, sometimes they are coming from nutrient deficiencies, and sometimes they are coming from mental restrictions.
Michelle [01:01:06]:
So I believe that your experience is real for them. And the way to target it is like we always talk about almost every episode this season and in past seasons is nervous system support is paramount so that you can start to understand what your body needs. And then honestly in the most transparent way. You just have to do things that you know are good for your body sometimes and let your body end up guiding you after. Sometimes we have to take action first and then our body can communicate better with us instead of first jumping into intuitive eating or what our body is trying to communicate with us. Because the signals might be very wonky at first.
Nicki [01:01:44]:
And I think too as you’re doing that really just and again, this is way easier said than done, but focusing on it from an additive mindset. So thinking about what can I add that will give me extra nutrients versus what can I take away? Because we know that once we start thinking about what we’re restricting, that’s when we start to get into that territory where it becomes a lot harder with thinking about food more and our cravings are increased. The other component too that I wanted to mention is if you can’t distinguish between hunger and appetite, if we’re talking about these two words and you’re like, I don’t know what’s what, I feel like they’re both the exact same. Start to journal after you’re eating. So I find that sometimes in that moment beforehand, it’s really difficult because things feel a little more urgent. So just journal what each feels like after you’ve eaten. Was that more of a physical hunger? Was that more of an appetite or an emotional hunger? And as you start to journal what these things feel like in your body, you’ll start to put those pieces together and make those connections which will then help you in the long run.
Michelle [01:02:47]:
Absolutely. And I just want you to leave with hope from this episode. I know that we’ve laid out a lot of physiology, a lot of the mechanics of this, and I also want to say that if you’ve noticed that you’ve done intuitive eating and that maybe the food chatter was decreased but you feel like you’re still craving those other foods, that’s okay. If you feel like intuitive eating was enough for you because really the cravings were coming just from a mental restriction, that’s great too. So every single person is going to need a different tool set. But it’s okay if intuitive eating hasn’t been enough for you. And it’s also okay if the physical changes that you’re making haven’t been enough for you too. If you notice you’re eating a diet that’s more composed of real foods, but you’re still having those intense cravings, it might be that mental restriction piece.
Michelle [01:03:32]:
So it’s really important. And this is the main premise of quiet the diet is that we’re looking at things from a functional nutrition perspective and also a compassionate body positive perspective. So how do we take both at the same time? And understanding appetite really comes from both places and just also, of course, if you’re feeling like your appetite is too low or your appetite is too high to just remember to breathe into that and non without whatever way possible, becoming so reactive to it because that can also then lead to other alterations. Really being curious around your hunger and appetite, as opposed to being judgmental or fearful. I know this is easier said than done, but we’re just giving you these very, very high level tips. I love that suggestion, Nicki, on what people can do to journal. And the other piece of it that I know we’ve brought up is if you can’t quite understand your own signals, even with journaling, even with intuitive eating, even with making diet changes, you can use trackers of some kind. Again, a continuous glucose monitor to give you a little bit more insight.
Michelle [01:04:30]:
I love my aura ring. You can use other tools if they’re accessible to you and you want them to better understand your body. Because if we were working on a really simple and clean slate that was even for everyone, and we were at a place where we were all, like, living in caves and hanging out with each other, I’d be like, it’s really clear what our bodies need, right? It’s really clear to understand. But as time has gone on, food processing has gone on, we have so many different things that complicate that relationship. It’s okay to use any tool you need to better understand. And again, don’t be afraid of your appetite. It’s a very healthy and good thing to have an appetite. And if your appetite feels too strong, there are many things you can do to experience it and release the tension of it and then also ultimately transform it.
Nicki [01:05:17]:
I’m just now only thinking about, when is this retreat happening where we’re all sitting in a cave around with each other. That sounds fabulous.
Michelle [01:05:24]:
I know. This is like, my ultimate dream in life, is to open a wellness facility where we could all just literally be, like, live in our evolutionary biological ancestors. That would be so amazing. Except with modern fun science, too. Both of it. All of it. Yeah. That would be magic.
Michelle [01:05:41]:
I know. We’ll do it. Nicki that’s the quiet. The diet center, it’s going to be called. Thank you so much, Nicki, for your Bang scientific studies this episode. We cannot wait to see you all for episode three.
Nicki [01:05:53]:
I’m so excited. Always love to be on the pod. I’m so glad you guys and the rest of the season is amazing. Can’t wait. Whoo.