Season 1 Episode 10 of Quiet the Diet Podcast with Michelle Shapiro, RD
How to Be Your Own Health Advocate with Andrea Nakayama, Functional Medicine Nutritionist
In this episode, Michelle sits down with Andrea Nakayama, Functional Medicine Nutritionist & Founder of the Functional Nutrition Alliance to talk about how to be your own health advocate.
They dive into how to navigate medical appointments and get the most results from them, despite the biases that many people experience while in appointments.
You’ll learn about how to navigate conventional medical appointments as well as functional nutrition and what it truly means to be your own health advocate.

They discuss:
- Functional nutrition
- Why you might leave the doctor’s feeling unsatisfied
- How to decipher our bodies’ signs/symptoms
- How to be your own health advocate for yourself in medical visits (step-by-step)
- Medical gaslighting – what it is & how to heal from it
- Case study: Hypothyroidism – standard vs. functional medicine treatment
Subscribe to get your weekly dose of NYC-style-sarcasm, nutritional nuance and messages of healing.
I know I don’t have to tell you this but this episode is only for educational purposes. It is not nutrition or personalized medical advice. We want you to get the most from the ep
Free Resources to be Your Own Health Advocate
Michelle Shapiro
I am so excited to bring you today’s episode not only because I have such an incredible guest for you. But also because the topic is something that is so near and dear to the work that I do to my heart.
And that’s probably because it’s also just a really frustrating experience that people have, which is the experience of going to medical appointments, whether that is in a nutritionist office, a medical doctor’s office, a functional medicine doctor’s office.
I receive on a daily basis, the sentiment from my clients, from friends and family members, how devastating it is when going to a doctor’s appointment, and leaving not only without the answers that they’re looking for, but with additional trauma and feeling like they’ve been gaslit and feeling like they are no closer to getting an answer to what they’re looking to accomplish.
I think that this feeling of going to an appointment, and having hope and really, you know, begging someone to help you and again being met with resistance or condescension can feel so defeating and so defeating that it’s it’s actually dangerous for people when it comes to their health. I think the approach that I’ve been seeing recently when it comes to medical gaslighting and encountering trauma and these appointments is really from a weight perspective which the damage of weight bias in healthcare also cannot be overstated.
I’m going to link a blog entry that kind of talks a little bit more about that. And one of the solutions that’s been proposed that I see a lot online and that I certainly agree with is to just ask the doctor not to weigh you to start with.
While this can be really helpful to limit the trauma that you may encounter from the appointment, you may not be getting what you need from that appointment still. So that’s kind of one approach, which is how do we limit the amount of potential triggering potential fear going into the appointment.
And then what I wanted to bring to everyone in this episode today is what you can do to prepare yourself for any appointment you’re going into because at the end of the day, you know, a vast majority, if not every single health care provider is there to authentically help their patient or their client.
So the kind of language between the patient and the practitioner needs to be bridged. And we have to create better connection and communication between the patient and the doctor, the patient and the dietitian or health care professional. If we go into these appointments on guard, knowing or thinking that this practitioner is not going to help us it’s going to set us up for failure as well.
And while the current model of medicine may be challenging for people with chronic illness, there’s certainly a right time and place for acute illness, especially in you know, emergency situations. So I think we need to appreciate the amazing benefits of modern medicine as well as the amazing benefits of Eastern medicines. And I think that we have to learn how to interact with practitioners so that we’re not going in and immediately either one of the parties are feeling threatened, unsafe, or like they can’t collaborate.
So this episode, we really are aiming to give you specific tools of what’s the best way to bridge that communication between practitioner and patient, how to create as much success in that relationship and as much success in your health goals in every single appointment, I could never have this discussion without my amazing guest, who is Andrea and Akiyama, she is the founder of the functional nutrition Alliance.
And for much of her career, she has been credentialing and certifying practitioners and functional nutrition. She is, in my head, a thought leader and in many people’s heads in the realm of not only the conditions themselves when it comes to functional nutrition, but the approach of the patient practitioner relationship, and really what Andrea would would also call kind of the art of the story, and how important our past and medical history is, in understanding our current medical status.
And Andreea is a beautiful storyteller. She’s an educator, she’s a teacher, she is one of my favorite people in the entire world. And we have so much to learn from her here too. I also wanted to let you know that if you are someone who’s looking to become a functional nutritionist, Andrea’s program, I love, it’s my favorite functional nutrition program. And I’m an affiliate for that program. If you were interested in learning more about full body system, by functional nutrition Alliance, we’re gonna link in a an affiliate code.
And again, the frameworks behind this program, I think, is really incredible. And this is speaking specifically to people who want to become functional nutrition health coaches, we originally filmed this episode and had to refilm it because Andrea and I are two people who get so impassioned by topics, we go way into the weeds. And we came back to this episode to kind of draw it back.
And we really wanted to give you those tangible, really easy to use tools of what you can do to prepare yourself before, during and after medical appointments, again, without creating that kind of feel of threat from either side. And in addition to that, you know, a lot of the work that I’ve done in my career is either I work with clients, one on one to help achieve nutrition goals.
And there’s kind of another leg of my business that I’ve been really excited about, which is helping patients clients to find the best functional practitioners and to give you tools on how to approach every single medical appointment, I have had originally started this as a membership, it is now a free, totally free membership for you to join.
And what’s inside is all of the tools that I’ve gathered over the years to find the best practitioners and the exact papers you should bring to track before you’re going into appointments and the exact tools you can use to make every single appointment as productive as possible and to get the most out of every single one.
I also have some awesome what I call wellness perks in there, which are just some free or discounted services to some of the best functional practitioners in New York. There’s a lot of virtual practitioners on there if you’re in other parts of the country too. And we hope that you enjoy that membership.
Also, because the buck doesn’t stop here. When it comes to learning about how to best interact in these appointments. Another free resource for you, is how to kind of track your signs and symptoms before going to appointments. And we’ll talk more about that in this episode.
Let’s get you freakin ready for your next medical appointment. Let’s get you ready and getting the most out of every single appointment that you have.
Intro to Andrea Nakayama, Functional Medicine Nutritionist
Michelle Shapiro
Today’s episode of quiet the diet is, I think, going to be my favorite one. And we didn’t even do it yet, because I’m here with my dear friend, one of the OGS of functional nutrition and one of the people who views every single person for their individuality their soul, but applies a really strong clinical basis to every single thing they do. My favorite human Andreea Nakayama Andreea, I’m so happy you’re here today.
Andrea Nakayama
Thank you so much for having me with you. I’m super excited, Michelle.
3 Primary Tenets of Functional Nutrition
Michelle Shapiro
So Andrea and I have a problem, which is that we can talk about, we have altered I have a million problems, one of those million problems is that we can talk about any topic. So deep down and dirty and inside the topic, that we can almost lose sight of the higher picture when we’re explaining it to other people.
So we’re going to be very intentional, this recording to give you really tangible tools, and at the same time talk about these heavier concepts that really come up for both of us and our functional nutrition work. And Andrea works differently than I do because she has more years of experience and a different pathway. So Andrea, can you just give us a little bit of an intro to what you do the work that you’re doing? And your story?
Andrea Nakayama
Yeah, thank you, Michelle. So it is very true, you and I can get very deep and in the weeds and in the branches. At the same time. I’m a functional medicine, nutritionist, and I started in practice working with clients. And that grew through lots of online programs to actually training other providers.
So I’ve trained over 7000 practitioners, so coaches and clinicians or those who are wanting to be coaches or clinicians in functional nutrition in over 68 countries over the last decade. And what’s so exciting now, in addition to the clinic that we have at the functional nutrition Alliance, and the training that I offered to practitioners, is that I am really turning my attention back to the patient in the books that I’m writing in the bugs that I’m writing and the speaking that I’m doing.
So it’s really important for me to empower the patient to be a real partner in their healthcare and to really dissect what that actually means. So to answer your question, in brief, I’m a functional medicine, nutritionist. I’m the founder of the functional nutrition Alliance. And I’m really starting to turn my attention back to the patient, which I’m super excited about,
Michelle Shapiro
and the basis of all the work you do for people who don’t know Andrea. If you don’t, I would be very surprised. But if you don’t know, Andrea, the basis of all the work that you do is around the experience of the patient and clinician relationship and how that really is an art and how it molds the experience of the client or the patient, and actually can be in and of itself powerful for healing.
Can you talk about that a little bit how important the practitioner and client or patient relationship is?
Andrea Nakayama
Yeah, so in the foundations of a functional practice, a primary tenet, and there are three primary tenets that I always return to is the therapeutic partnership. And the therapeutic partnership is really cultivating what I like to think of as functional empathy. How do we understand not just what you’re experiencing the pain points, but who you are experiencing them.
And this gets back to my story that you were asking about. So I lost my husband over 20 years ago to a very aggressive brain tumor. And he was diagnosed in April of 2000, when I was just seven weeks pregnant. And that was a real wake up call for me because it was the first time in our 30s at that point that we were really exposed to the medical institution. Really, what is it when you’re dealing with a chronic and life altering diagnosis, and so a Somu, my late husband was given about six months to live, we were ultimately able to keep him alive about two and a half years, so he wasn’t expected to see our son born and ultimately had a good year and a half of imprinting.
But that time for me woke me up in relation to what that therapeutic partnership is or is not depending on the relationships. So I saw Isamu treated like his diagnosis alone. And I think we’re so accustomed to this when we’re seeking answers, that that’s what we go in and talk about, we only talk about our signs or symptoms or our diagnoses, but two people with the same signs, symptoms or diagnoses got there for different reasons, those things are just the tipping point. And so for me, really recognizing, who are you that’s experiencing, This shifts the entire relationship healing process like you’re speaking to, but also the trajectory of care?
Michelle Shapiro
Absolutely. I think that when we think about the modern medicine model, it’s these, you know, again, especially in the case of glioblastoma or brain tumor, we think about more solutions based more, we have to fix this problem, which in some cases, as we both know, is completely essential.
And absolutely, and then the functional nutrition side of things is a little bit different. And I want you to talk through that. But I’d be remiss if I didn’t mention that a cornerstone of Andrea and I’s friendship and relationship has also been that I had a family member who was diagnosed with glioblastoma, brain tumor, a stage four brain tumor, now 20 months ago, and had the same prognosis and Andreea
Amazingly, this is just a spiritual an important piece of this conversation, amazingly, has been was so so supportive this entire time, and which I attribute to why my family member has been so successful. Which, again, is there any success in any of this? I don’t know if that’s the right word, but she is feeding odds, I guess you would say was one of the reasons is that Andrea set me up with a functional nutrition team to support her who specifically works with this cancer.
And what they do is they support not only using modern medicine and chemo therapies, but they show us as the client, how to target the chemotherapy to make it more effective using nutritional supplements and how to keep the body healthy at the same time, which I feel is very incredible in something totally different. Because normally we think of functional nutrition as being very stratified between it’s either a dichotomy, it’s either you know, Western medicine, you can only get chemo or you can only do weird herbs, you know, that people are thinking of. So it’s interesting that our personal worlds aligned.
I mean, we don’t believe in coincidences like that. I know, I know, we were brought into each other’s lives for a lot of reasons. But it’s also interesting how I think this explains a lot of what I believe true functional Integrative Nutrition is, which is bringing in all different worlds. And like you said, in your journey with the SAMU, you were willing to try anything. This was what sparked your interest and saying, Is there any more methods available, and also, the fact that Osama was in these appointments, and people will look at him, and really, from what you’ve explained to me write him off.
And I know, I’ve experienced that, as I go into all of these medical appointments with my family member, I find myself advocating not only for good care, but also for them to view my family member who’s one of the most important people in my life as a person, not just a diagnosis.
What is Functional Nutrition?
So can we talk about just way back? Yeah, what is functional nutrition mean to you? And then we’re going to talk about how we apply that within the relationship and a doctor’s office. But what does it mean to you functional nutrition?
Andrea Nakayama
Yeah, so for me, it’s really about the Yes, and. It’s about understanding the person’s story. So in functional medicine, functional nutrition, these are called the ATMs and ATM stands for antecedent triggers and mediators, their soup, as I like to call it, which means everything that’s going on in their body, and their skills, who they are and what they’re doing right now. So I’m going to go back over each of those, but just to say that it’s the Yes, and.
It’s not my job as a functional nutrition counselor, to address Esau moves brain tumor, or anybody else’s to more or diagnosis. It’s my job as a functional nutrition counselor to shift the terrain in which that diagnosis is occurring. So in that way, we shift the odds, we shift the prognosis we can even alter the course of the quote unquote disease, because that disease exists in an environment and our job in functional nutrition is to change the environment. So that’s an easy way of thinking about it.
Antecedents, Triggers, and Mediators
But we do that by looking at the whole. So when I talk about their story and their antecedents, triggers and mediators, antecedents are everything from how were you born? Were you breastfed? What birth order were you all of those things actually make a difference in what led us to where we are today and our outcomes, nothing is right or wrong.
They just help us clinically from a functional perspective, understand what we’re working with in the individual. Our triggers can be emotional, they can be physiological, they can be physical, a car accident, stress when your parents got divorced or when you went through graduate school or in a job OB, they could be food poisoning or exposure to a virus or a bacteria.
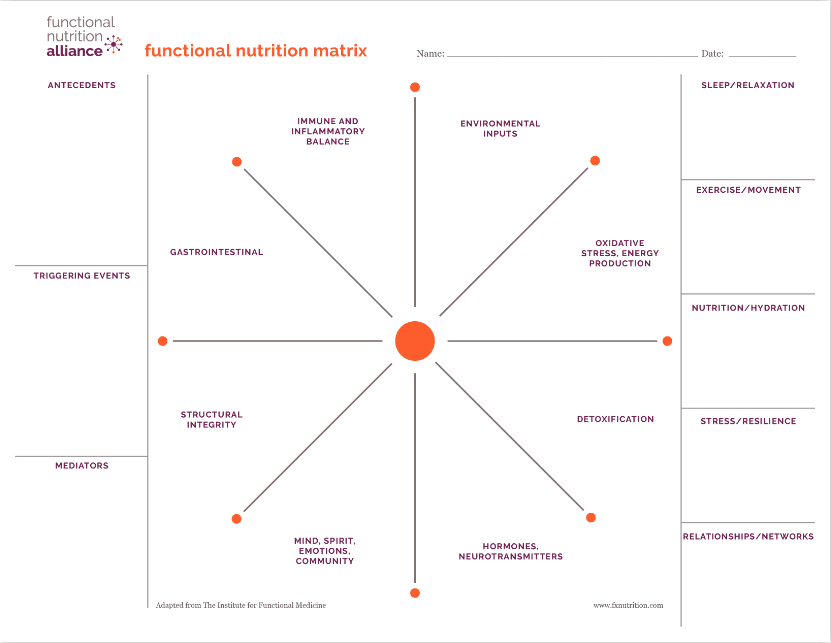
So triggers are many things that help us understand, oh, this is who you are and what got you here, we’re just looking at the tipping point. And mediators, Michelle are my favorite because they’re related to the right side, or what I think of as the skills on the functional nutrition matrix. And I think through the Functional Nutrition Matrix, which we can talk about, but the mediators are what make us feel better, and what makes us feel worse.
And this is something we can all ask ourselves, and really anchor on because it helps us to take better care of ourselves when we recognize you know what, when I go to sleep at 930, I actually have more energy the next day, and I’m struggling with energy and fatigue issues, how do I make that a priority, or when I drink coffee on an empty stomach, I noticed that I’m more reactive during the day little things that we can start to pay attention to. Those are our mediators, they’re part of our story. They’re part of our reality, and they’re ours to work with.
Michelle Shapiro
Absolutely. And I think I’m going to reiterate what you’re saying, like, please, it’s so important, which is that everything that you are and have done is important, and a part of your health. Everything that you feel is important and a part of your health.
So again, we can be having a conversation about current gut issues. And we want to know what happened 30 years ago, yes, how we’re going to know what’s happening now. So to understand that our bodies are constantly reflecting what we’ve been through and constantly changing as a result of what we do and what we eat is so important and how we feel is so important and influences more of how we feel physically.
I think that that concept for people to understand, for the work you do is essential, because again, for the Westerner, every single part of your health history and your life history is important for a practitioner to understand before making a recommendation.
So this Andrea, the functional nutrition matrix, specifically, your interpretation of the functional nutrition matrix is not what we see in modern medicine, right? Generally, what people are experiencing is walking into a doctor’s office, potentially feeling intimidated to do that, and leaving with some sort of prescription after a short time with a doctor.
I want to first ask you, because I like you believe that functional nutrition and medicine at its core is the move. I think it’s the right move. And it’s the vibe. Tell me why is there such a divergence? And why is it that we have this experience in modern medicine? Now, why do people feel this way when they leave appointments? Like can we talk about how that ended up?
What is the Difference Between Functional and Conventional Nutrition?
Andrea Nakayama
Yeah, I think that there’s a lot of different reasons. And I think our modern medical system is anchored on acute care diagnosis and treatment. And so that is where we know what something is we can label it. As patients we feel relief in the label, even if that label doesn’t bring us all the relief we need. Because finally something has a name, we get a prescription or a protocol.
So I think that functional medicine is at fault in this as well. So get a prescription or a protocol, we leave you thinking it’s going to be fixed. And that is not the case. And that is because this way of thinking is for acute care if you have a broken arm, or your heart isn’t working or something is very acute that needs to be addressed. That’s where our medical system has evolved to be, frankly, quite brilliant.
There’s more and more that can address that acute care diagnosis with treatment. When we get to chronic care. That’s where we’re missing some key pieces of how we even think through a problem. Dealing with chronic care is like going into the abyss because we got there for different reasons, ie somos brain tumor, and your family members brain tumor, same name, but they may have different activators that are causing them to grow. And that’s where we go deeper into understanding. Why is this happening? Not just what do I do about it?
I have Hashimoto’s autoimmune thyroid disorder. If I look at any of my colleagues who have written all the books on thyroid issues, and I know them personally, if we look at the fact that we both have the same diagnosis or we all have the same diagnosis, we Got there for different reasons, to people with breast cancer may have different things that are activating their cancer and more and more areas of progressive science research are helping us to understand this individuality, but it hasn’t made it into medical care. So in traditional medical care, we need it like it is for the acute care surgery.
Michelle Shapiro
Goodness, you break a limb, please. Yeah, like, take me to the ER, not a question. Exactly, exactly. Yeah.
Andrea Nakayama
And when it comes to chronic care, we’re at a mismatch. And that mismatch is the system of medicine. But it’s also how we as patients, think of our health and what we’re expecting out of the people that we’re seeing for quote, unquote, treatments.
Why are Chronic Illness Rates So High?
Michelle Shapiro
Absolutely. And when we say chronic illness, give me some examples of what are some, maybe, let’s call it Life driven chronic illnesses. I don’t like the word lifestyle here, but like life driven, chronic illnesses that you’ve seen people facing and are common that you see.
Andrea Nakayama
Yeah. So when we say this, and we say that they’re lifestyle driven. That’s what tends to be said, it doesn’t mean you did something wrong. to reframe this idea that we’re broken. There’s the field of science called epigenetics that helps us to understand life influences, and those life influences start from before we are born, there is cultural heritage thing, things we’re carrying in our bodies, whether our families were enslaved or lived through famine, those things actually shift our genetic makeup and therefore the expression of disease.
So a chronic disease is one that is where we’re sick and not getting better, basically, and easy terms. And we can’t find the easy solutions. No matter how many people we see, no matter how much research we do online, but diabetes is going to be a chronic health condition, any mental health or Alzheimer’s, that’s a that’s a chronic condition, all autoimmune conditions are going to be chronic conditions.
And those are affecting more and more people, there’s 10s of millions of people 75% of whom are women, and more and more of our girls are experiencing a shift in our immune system that’s turning on itself and attacking our own body. And that is a chronic condition, because we have to think about it differently than just taking a medication to squelch the physiological or biological reaction. And
Michelle Shapiro
so what you’re saying is also if a condition came from an antecedent and a trigger, influencing it, you’re not going to work your way out of it by taking a medication or supplement, because you have to understand where it came from, to be able to treat it is that exactly,
Andrea Nakayama
and otherwise, we’re saying it’s like whack a mole, right? If we only suppress the symptom, and we don’t look at the why it’s going to manifest elsewhere. And a new symptom is going to arise sometimes new symptoms from the medication, and sometimes new symptoms from the biological problem that wasn’t actually addressed with the suppression of the symptoms. S
o this is where we get into what’s called polypharmacy. We’re playing Whack a Mole. And we’re not actually addressing the underlying reasons why something might be at play.
Michelle Shapiro
You say whack a mole, I say Pop – a – weasel, which I think is something which is like one thing goes down, another thing comes up, basically. So this idea, by the way, that symptoms, when you suppress them might create new symptoms for people. It’s also something new that some people might be listening to and saying what?
What is Patient Advocacy?
Michelle Shapiro
So what I think of our symptoms, and we’re going to talk about the difference between signs and symptoms, and all that fun stuff, too. When I think of symptoms, I think of, you know, we think of discomfort and things that we don’t like, I think of it’s a communication system between our body, our brain and basically trying to give us a message like, hi, I need you to focus in words. What do you think about symptoms, you know, as messengers and tell us more about that?
Andrea Nakayama
Yeah, absolutely. I think symptoms are our biggest clues that we can tap into and tune into, to see how are we feeling? And again, back to those mediators, what makes me feel better, what makes me feel worse.
And when we have that kind of data, we’re able to advocate for our health differently when we do see our providers. I just as an aside, I think we think that patient advocacy and standing up for ourselves means going in with our hands on our hips and kind of like yelling at our doctor and telling them what we want.
But patient advocacy is really about knowing yourself better and being able to communicate that, that’s when a doctor shows up differently because they know you’re paying attention to what only you can pay attention to. And that’s really different. When we think about the opportunities, their symptoms are a huge opportunity, as you said, Michelle, to tune in to pay attention, and then to be able to express what’s actually happening to those who are there to help us find resolutions.
Michelle Shapiro
Absolutely. And I think about those symptoms, let’s use anxiety as a symptom, right? So anxiety is showing up. And I use the metaphor that anxiety is like the fire alarm in your house. So if you had a fire, right, we wouldn’t want to have no fire alarm going on. So I think a lot of times when it comes to anxiety, we want to take a medication and make it go down because we hate it and it’s uncomfortable.
But then we’re not going to know where the fire starting. So it’s really important to listen to and experience and work with your symptoms. But I think the magic of the practitioner is being able to take those symptoms, and put the puzzle together of what’s going on.
So I think when it comes to like you said patient advocacy, I think a lot of people think they should walk into the doctor’s office with I looked up histamine intolerance, and these are symptoms, walk in with your signs and symptoms, not your solutions. And I think that’s really important for patients to hear. What’s the difference between signs and symptoms also tell us that?
The Difference Between Signs vs. Symptoms
Andrea Nakayama
Yeah, so this is something I think is really interesting for us to think of as patients when we’re thinking about advocating for ourselves. So our medical providers are very anchored on signs. These are things they can measure, they can measure a fever, or rash, something they can see or measure is a sign.
Our symptoms are the things like the anxiety, the fatigue, the discomfort, that we have the GERD that’s not necessarily something that they can measure. So we have to express it, and be able to speak into it. So one area of advice I would give to all patients in terms of advocating for themselves is no your signs, they can measure it versus your symptoms. They can’t see it, but I feel it and express them differently.
Because when we speak about our signs and symptoms in Confluence, we are short circuiting the brain of the person who’s like I got a measure that I don’t know what that is, I don’t know understand how that is, if you’re unconscious, your signs can still be read. If you’re unconscious, your symptoms cannot be determined.
Yeah, so that’s one area that we can go in and speak to the difference. When we’re also advocating for ourselves. If we can speak more thoroughly about our symptoms, again, not the solution that we’re expecting, which may be the supplement or the test, we often go in thinking like my I hear this a lot, Michelle, I don’t know, if you do my doctor won’t run my doctor, won’t I Roy labs, exactly. Iron lab, thyroid lab, that’s a big one, and then a ton of frustration with what the doctor won’t run.
So one thing I want to say there is doctors won’t run what they don’t understand. So what the doctor is telling you is I don’t know what to do with that test or those results. So I won’t run it for you. And Bravo,
Michelle Shapiro
actually, doctors have to be the one to interpret the lab. So if I, as a dietitian, also say to my client, can you get these labs down to a doctor’s office because dieticians in the state of New York can’t run lab tests, blood lab tests, then the doctor him him or herself specifically has to be able to interpret them. And that makes total sense, because you should not just give people labs and say, See you later, it’s actually helpful when they do that. I get that. Yeah, so
Andrea Nakayama
understanding the limitation of their scope as well helps us get out of that like fight that we’re often in with finding like who’s the person who’s going to be my be all and end all it may not be one person. So understanding that they won’t run something that they can interpret and can’t do anything with. And that’s where the limitation is and where that guides you is another story but it tells you this is where the limitations are.
How to Be Your Own Health Advocate
Andrea Nakayama
The other thing that I want to recommend is how you show up and be your own advocate given your health symptoms. So if we’re able to say let’s say in relation to anxiety, two things that I want to say here, one is showing up and letting the doctor and the staff know hey, I suffer with anxiety. This is how it’s going to show up in my medical visits. I might kind of have to now when something is being talked about that scares me and then I’ll probably go home and go on Google and start driving myself crazy. Can you hold that with me? Can you hold that awareness with me that that’s what might happen as you begin to speak to me.
So asking for that help up front is very, very helpful. Number two is to know the history of that symptom. So being able to say, I suffer with anxiety, I’ve had it since I was 13 years old. It started when I was in the spelling bee, and my parents were getting divorced. Like being able to succinctly speak into your history with it, I’ve noticed this is what makes me feel better. This is what makes me feel worse, whether they dismiss it or not, you’ve gone in there displaying and showing your self awareness.
And I will tell you, doctors respond to you differently, when they know they’re talking to somebody who is taking notes who is aware of their situation, they’re going to rise up, when you’ve risen up, and you’re not rising up in terms of telling them how to treat you, you’re rising up in terms of telling them about you, because you’re the only one who knows that.
Michelle Shapiro
And in the most unfortunate way, we do know that practitioners have biases, and ones that are coming up a lot recently, or weight biases. So coming in with this approach, also will help the patient no matter what, right.
So even if someone does have weight biases, this is still advocating for yourself, in a the most still respectful manner possible, but still with the confidence of knowing yourself which every single person knows themselves better than any practitioner ever, is still going to get you better results.
How to Advocate Against Weight Bias with Your Doctor
Michelle Shapiro
But in some cases, it might not get you the full results talk to me about in the devastating and frankly very frequent scenario, that there is a huge weight bias. And let’s say someone in a larger body goes to an appointment, and you know, is complaining of symptoms that we’re talking about. It could be something like anxiety, it could be something that’s more of a sign like a rash or something like that, a combination of signs of symptoms, and the doctor insists on only talking about weight loss and weight loss prescriptions. What kind of advice would you give to a patient of that scenario?
Andrea Nakayama
Yeah, and it’s, I think it’s, I just want to really feel the challenge there. Because I think there are more and more people who stopped going and seeking support because they don’t want to hear the same diatribe. And that becomes really difficult because people aren’t getting the help that they need for other things that could be contributing factors that could be completely other than.
So I think that it really depends on the individual and what they are experiencing in their body and in their embodiment, and how they go in and recognize what it is that they’re asking for. So being able to speak up and say, This is what I’m working on. I know you’re gonna say this, to me, this is what I’m here for, I’d prefer if we focused on this aspect, an issue that I’m bringing forward to you today.
And continually bringing it back and recognizing that may be hard as hell to continually say, I know, we spoke about this, and I’m asking that we focus on this rash, I am working on these things. It’s not what I’m here for, instead of the feeling of being gaslit that you’re not being heard. It’s hardcore, but I think it is what we have to do and how we have to really speak up for ourselves.
And walking out of that appointment may feel frustrating, but at least you did good by yourself in whatever way you can. And again, the question you’re asking, Michelle is so complicated, and it’s gonna go no different for each individual. And it may also be bringing somebody with you to the appointment for your rash or your migraines, and being able to say what that is that you’re asking for.
And then have the other person say, Hey, I know that they said that they want to focus on we’re already working on that. So really, let’s focus on this because that’s why we came here have another health advocate with you.
I know even if we go back to the situation with my late husband, the SAMU. There were times when I wanted the doctor to speak to him he was perfectly capable of speaking to them. And there were other times where he would say Andrei is going to be my eyes and ears today. I can really I’m a little foggy brained because of the chemo or the radiation or whatever it was. So bring somebody with you. It is totally okay to not have to enter those situations alone.
Medical Gaslighting & How to Advocate for Yourself
Michelle Shapiro
I think having a health advocate is really, really helpful for somebody People and then again, if you feel emboldened yourself to anyone listening to go into those employee appointments and advocate for yourself and your health, that’s amazing too. And we’ll give you some tools on how to prepare that.
I think that from an emotional standpoint, it is completely heartbreaking to be asking someone for help with your health and a vulnerable situation and to advocate and be met with dismissal and gaslighting, especially to be judged for your wholeness and your, who you are as a person and your worthiness of being helped. Based on external factors. I know it can be legitimately extremely destabilizing for people.
And I just, you know, I personally have been in that situation. So many times, when I grew up, occupying a larger body and had doctors write me off, treat me differently. And as a young person, it was really, you know, quite challenging, I would say.
And I also want people to, from an expectations perspective, understand that this may be the case but not anticipated and not, you know, necessarily put yourself into that fight or flight mode going in. And kind of removing your identity and who you are from the reaction that you’re getting, knowing that it is a possibility, but that you’re walking out of the appointment, the same amazing person you were when you were walking into the appointment.
And if you need to do something really soothing after that’s totally fine. But I would say the strategy of going in with expectation, but not anticipation that something will happen but at the possibility and going in a little bit, you know, vulnerable with this information.
But again, understanding this can happen is really important for people and also just making sure your nervous system as much as you can do some beautiful breathing, have an ice bath before, after anything you need to do to really access you know, your nice parasympathetic nervous system and really soothe yourself as I think totally, totally helpful to
How to Heal From Medical Gaslighting in 3 Steps
Andrea Nakayama
Yeah, I mean, I think one of the ways that I look at medical gaslighting, which can happen in big ways and little ways. And I have another thing I want to say about bias is that we have to really recognize that whatever happened is not our fault. And under all, whatever went on in that appointment that made you feel unseen, unheard is a result of the lack of that therapeutic partnership that we started this conversation with.
Those biases can be really overt in ways that we’re talking about when it comes to body size and weight. biases can also happen when we’re seeing a provider who thinks through a very specific diagnostic lens, whether they are always looking for adrenal fatigue, always looking for small intestinal bacterial overgrowth.
Always looking for h pylori, we can find these cracks and crevices in any case that we’re looking at. And I know I’ve been in situations where the biases of the provider made me feel like they were placing a diagnosis on me that wasn’t appropriate for me. And then I’m supposed to do some whole protocol that then doesn’t make me feel good. And that’s another form of medical gaslighting.
So I just want to recognize that it occurs in all sorts of ways that if you leave an appointment feeling like that felt bad, I did not feel seen, I did not feel heard, I did not feel taken care of that.
- It’s not your fault, now more to consider what your options are. And we may have options to switch providers, you may not have an option to switch the office that you go to, but you may have an option to switch the provider within that office. And you can do that. And that is something I think we don’t often we feel like we’ve been assigned somebody. And that’s what we’re supposed to do who we’re supposed to see
And it’s totally okay to advocate for yourself by calling up an office and saying, I met with Dr. So and so it didn’t go well for me Are there any other providers who work with XYZ, they’re going to care about your experience and want to hear that and then you can go into that next appointment and say I met with Dr. So and so they’re perfectly nice, but this is how I felt I’m looking for a different experience. - And so I just want to bring in that point number two, which is consider your options fully my number three and that healing from medical gaslighting, so number one, not your fault number two, consider all your options to move forward.
- Number three, is that take care like actually take it, do the soothing talk to whoever you need to talk about. This is your opportunity to say that didn’t work for me and develop your parameters around what you know will work. It’s like dating, you know, like, you need to find the right persons. Yeah, absolutely. There may be more than one.
Michelle Shapiro
Sure, but we just don’t. We would find a way out of your life, you know, have fun. Exactly. Exactly. No judgement in this podcast. I’ll tell you that right now. Exactly. I think the idea that people can be their own, you know, you’re hiring basically a consultant to help you with something right to know that this is where your money is going, where your hope is going all that, that’s for you to choose completely for you to choose.
Obviously, there are limitations due to locational areas, thank goodness, a lot of practitioners can see us virtually now, which is really awesome. I developed a tool specifically for this to help people find different practitioners, it’s called Wellness map, you can check it out wellness map taco, to help people find different practitioners who are compassionate, we’ll look at people as the whole picture. But it’s not its location and financial totally, you know, dependence. This is there’s definitely limitations for that.
So I’m going to bring us back just through kind of the patient client experience and how people can get the most out of all of their doctor’s appointments. I also have a free PDF, how to leave your doctor point without feeling like crap, Andrea has a tremendous amount of resources to that we’ll talk about and how people can access them.
How to Prepare for Your Doctors’ Appointments
Michelle Shapiro
But step one, and I kind of want to walk through like a little case study with you, Andrea, if you don’t mind, I’m going to make up a person and tell me how you feel they should best prepare for the appointment, that they’re going to find a practitioner and what what it would look like for them.
So this person has a diagnosis of hypothyroidism, they notice they have symptoms like their hair has been falling out, their hands have been cold, they have some weight loss resistance. They have been to practitioners who have told them weight loss is bad for your relationship with health. They’ve been to practitioners who put them on thyroid medication. And at this point, nothing’s really making them feel better. Yeah.
So what would be the steps they should take? And ways of preparing for an appointment with a new professional? And, you know, take me through the planning phase of that?
Andrea Nakayama
Yeah. So that’s a great question. And I think we see many, many of these people Oh, yeah, even if they have received a diagnosis that there’s the recognition that the diagnosis does not lead to the quote, unquote, cure, that sometimes the diagnosis is just another set clues. So my favorite tools to use for preparing are tracking tools, the more we can track and understand what is true for us.
Again, I’m going back to those mediators, the more we represent our history, and what’s occurred for us. So for me, there’s all different sorts of tracking, there’s tracking at what we eat, which is not helpful for some people. So we may need to put that one aside. But being able to look at if you’re able, what it is that you’re consuming, and if you notice that it makes any difference or not is a great way to advocate for your own health.
Again, some people are really triggered, I don’t like the word triggered, but like they’re triggered by doing that. So if we have to put that aside, that’s fine. We can track our elimination or our poop. So just looking in the toilet and knowing like I’m pooping once a day, or I’m noticing my metabolism is slowed.
Pooping is going to be impacted by the thyroid because it helps with our metabolic function at a cellular level. So being able to say, I’m not feeling constipated, but I’m only going to the bathroom every other day or the opposite. Being able to speak into that is important, I noticed a difference.
When I started the thyroid medication, it led to more diarrhea like when we can make those connections between what’s happening with us, we are giving further information so that we’re not just layering things on top of recommendation recommendation, protocol prescription, we’re helping to actually bring or illuminate what’s happening in that environment.
And then any of those signs or symptoms. So tracking that we can also track how much we’re hydrating, we can track what our sleep is like we can track our menstrual cycles, there’s so much we can track that is helping us to illuminate a better story for the provider that gives them quick insight into what they’re trying to address.
So for me, the answer is always in the tracking track and in the understanding of this is what’s true for me. Otherwise we show up like any hypothyroidism patient who’s having all of the symptoms and the There’s no added information, there you are your diagnosis and not your person in that situation.
Michelle Shapiro
So even if you have a practitioner who does have a tremendous amount of biases, and is not looking at the people as a whole person, it actually forces the practitioner to look at everything. So again, without being run this lab for me, you’re actually saying, here’s all of me. So the practitioner can then make the choice to have bias, but you’re giving them a real opportunity.
And you’re making things a lot more easy in that relationship by just saying, Here’s everything that’s going on with me, I also can include a doc PDF below, which is, you know, either downloaded or you can make one yourself, which is just draw a body, and different lines on the body where you’re experiencing different things like near the head, it could be anxiety, or it could be headaches, like Andrea said, maybe you make one side of the sheet signs and one side of the sheet symptoms.
So if it’s something like I noticed a pain in my wrist, that’s going to be a symptom, if you notice that you get a rash on your wrist, that’s going to be a sign, just so that the doctor can have an understanding of you know, the signs is really easy for them. That’s the language they’re going to speak and symptoms might be a little more gray area. But I know if you went to a practitioner like Andreea, I, and you told us about a specific rash, we would want to know excruciating details about that rash, how long it’s been happening.
And what I want people listening to understand as a patient is that every piece of information about how you feel is essential to the treatment plan you’re going to be getting, especially if you’re working with a practitioner who’s listening to those details, I mean, the difference between a client of my waking up at 2:45am versus 3am, the difference between a client of mine sitting up while they eat or sitting back, every single tiny thing that you don’t think is even a big deal about you could be essential to cracking the code of the terrain of your body, basically. So it’s so important.
And again, I can’t express this enough how you feel and what you’re experiencing is the most important thing in the world. Don’t ever dismiss what you’re feeling or something you have. My cousin had a rash on her face. And it would happen at the same time every single day. And it was only until we realized the timing of it, why it was happening under times of stress that it had heat when he touched it, that’s when we were able to get a diagnosis because a diagnosis and ended up being diagnoses.
But from a doctor, because we came in and said, Here’s the details of that it makes it easier for the practitioner versus again, we have this idea of advocacy means walking into the appointment and saying I was on Google, about histamine intolerance. And that will really not get you far because you’re also taking away the role of the practitioner. And I know you like talking about this recently, too.
And I mean, again, um, the many things we talked about, we did speak about this recently, which is when people are also trying to become their own practitioner and their own doctor, and how do we avoid that pitfall? Tell us about that.
How to be a Better Patient
Andrea Nakayama
Yeah, I think this is where we’re getting confused with all the noise that’s on Google, or in the books or on social media, with what it means to as we’re discussing being your own health advocate. And what I see is that more and more patients are playing practitioner. And I have to say, even if we are practitioners, there’s some times that we have to do our work to be patient.
So let’s say in my case study group that I’m working on for my book, I’m constantly reminding them how to be a better patient. What does it mean to be a better patient? And it means collecting this information about yourself versus saying, Should I take the Candida cleanse? Should I do intermittent fasting? Should I am like, why are we even asking that question like what is wrong posture leading you to the recommendation before we have the proper assessment.
So sitting in the assessment is the way that we can be the best patient. And you know, Michelle, as you were talking, I was thinking back to the early days with the SAMU. When I wasn’t a practitioner, yet I was this. This was a career change for me after he passed away.
But we had our E Somu. Book, and we would go in and they would say when did the stigma happen in the eye and I could flip through and say it happened last Tuesday. And since then it’s been able and they would go okay, so it’s knew what and week I could speak into what changed during that time. That’s when we introduced this, that’s when you introduce this. So we had a deeper conversation.
And I have to tell you, every provider was not only impressed with the information that we had, but also ready to have a deeper conversation with us because they knew we were keeping the notes. And so that is in some essence what I think the work has evolved to for me and being a better patient.
It’s about really knowing yourself and what’s true for you and showing up with that piece of data so you know it It’s called, or we could think of it as patient centered data. It’s what we can gather that nobody else can except us. And there’s actually more and more researchers, female researchers who have chronic health conditions who are starting to go into that realm of what is true for the patient, because we don’t have the diagnostic tools or criteria for a lot of chronic health conditions.
And that’s really fascinating to me that researchers, female researchers who have chronic health conditions are starting to say, because we don’t have the diagnostic tools for these things, it has to go back to the experience of the patient, that’s going to lead to the evolution of the diagnostic criteria. And I know that’s a big concept to wrap our heads around. But it just speaks while the importance of the individual data and what it can illuminate.
Dealing With Bias in Healthcare
Michelle Shapiro
I still have to just hammer in this point, everything that has happened to you in your life has led you to this moment, for better or for worse, and who you are so important, all of who you are every bit of who you are. And the way to have people recognize that is by expressing it, that’s the way to have people recognize that and to treat you in that way. So what I don’t want anyone to get from this podcast is that, hey, the work is on the patient only to get a good experience.
The reason why Andrea and I both view it from the view of the patient is because we have more ability to empower you the patient than we do to change the medical system. The idea that someone could walk into an appointment, and I’d be treated differently because their weight makes me physically sick. Yes, someone being treated differently because of their race.
I mean, these are, it’s like any empathizing person, any rational person would be completely horrified by it’s horrifying, there’s no other word for it. That being said, how we can best help you with that is to give you the best tools possible to have an optimal experience, if we can’t change the entire medical system, which we’re we’re both really trying to, by the way, a lot.
We’re both trying to, especially from the nutrition end. But if we can’t do that, what we want to do is arm you with the tools of safety, and really efficiency, we want you to get the most out of every single appointment that you can go into.
But I just needed to say like, we’re very aware that you shouldn’t really have to be doing all of this. And that it shouldn’t not that you shouldn’t be having to advocate for yourself and your own health, but prepping yourself for disappointment and all that.
We really wish this wasn’t the world. But it is and this is the reality. So I’d rather give people the tools for the current reality as opposed to law of all lands, which is every appointment you go to is going to be amazing. It’s not Yeah, but you can make it as productive as possible.
And also just again, from an empathetic standpoint, man, do we feel you and man Do we understand what it feels like in the case of Osama and my family member, especially going into these appointments, to feel like someone is being treated like a diagnosis. It’s extremely painful and experience to not it’s like this is my part you don’t know Esau mu this is a sama you don’t know this amazing, brilliant man, like how do you not know this person, like I know this person.
So just to say, from an emotional standpoint, we totally freaking get it. And this is just so that you have the tools to make the most out of every single appointment. And actually, while you’re doing these tools, you’re learning about yourself. That’s the most amazing part is that totally don’t actually draw a puzzle or a timeline, as Andrea would definitely say of our lives all the time.
Yeah, we don’t get to sit down with ourselves like that. It’s healing to just even learn about yourself. So there’s always something you can get out of these tools. I would encourage people to do this and to track as Andrea says, anyway, forget about an appointment tells us something that’s really essential for us learning about ourselves.
Andrea Nakayama
Yeah, I mean, when we think again about those mediators what makes me feel better, what makes me feel worse if you just stop and think about that. And what are you unsure of? I don’t know, if eating gluten makes me feel better or worse. I can’t tell because I just feel worse right now.
So if you have your yes no maybe list in terms of those mediators tthat starts to be really revealing and leads to a different discussion where you might say you know what, I know it feels better. When I don’t drink coffee on an empty stomach. When I get up and stretch in the morning. I feel less body fatigue later on in the day, whatever it is, that is true for you.
You then have some things that become the area that you can focus on either to do or to even speak to someone like you Michelle about like I know that when I hydrate I feel better but I don’t want to because it makes me go to the bathroom all day long. And I’m teaching and I can’t get up to go to the that’s a different conversation that leads us to diving into what the appropriate recommendations are for you versus not knowing that piece of information, right?
Functional vs. Conventional Nutrition Recommendations
Michelle Shapiro
The difference between someone who doesn’t want to drink because they’re quote unquote, lazy, which I don’t believe is the case for literally anyone. I don’t think we do anything out of willpower or laziness. I think we do everything under these really, because of these really important features about us.
But again, knowing what Andrea just said, the difference between someone who says they can’t drink water all day because they have to teach and knowing someone who says they don’t drink a lot of water. Do you see? Now I know you do, Andrea. Listener? Listener? Do you see the difference between how that would inform a recommendation?
And the case of someone who says I’m going to the bathroom all day? I can’t because I’m a teacher, we might time it really perfectly. When you’re having that water? You know, we might specifically make recommendations based on that versus someone who says I just don’t drink a lot of water, then it’s like, well get your eight cups in a day.
It doesn’t warm the recommendation as much. Yeah, the minutiae is the magic. Yes, you might not think it’s important. But every juicy morsel as Andrea would say, of information is so important for the recommendations you’re gonna get. And again, it doctor’s offices are going to be different than nutrition appointments, where you get, you’re gonna get much more into the weeds.
But even like, let’s say, you know, I used to have anxiety, I was like, 18, right? I’m going to doctor’s appointments, and they’re like, Why do you have anxiety? And I’m like, I don’t know, I have no idea why I was because I had lost 100 pounds in three months, obviously, is why I was having anxiety.
But I would go and start appointments, and they would always offer medication solutions, but part of my anxiety was being afraid of medication. So if I also would have said, Hey, I can’t really have a medication solution, is there anything else we can do that informs the whole discussion? Because then I’m not leaving with a medication solution.
So whatever your boundaries are, whatever your signs and symptoms are common, knowing it and owning it, without having to own the doctor or without having to own the experience, own yourself. That’s how you get the most out of those appointments. For sure.
Andrea Nakayama
Yeah, I think just one final point. Michelle, what you just said about water is the difference between nutrition and functional nutrition, drink eight cups of water a day, eat fiber, those are nutrition recommendations.
Functional nutrition is what does this mean for your body’s function. And that’s going to be different for everybody. And you deserve each of us. Each of you deserve the opportunity to see where recommendations actually impact your body.
Michelle Shapiro
I don’t think people can understand how different functional nutrition versus nutrition recommendations how vast that difference can be and how big of an importance it is. Which is of course, the individualized nature, but it’s also focused on actually whatever the real problem is, right?
I think, for people to understand, again, that giving nutrition I hate like principled people and things I’m not I’m not like a morally righteous, principled person. I don’t care about what works optimally for people. If drinking eight cups of water is a principle, I don’t care about the principle I care about how do we get you drinking one more cup of water a day.
So that I think is also the difference between nutrition principles and nutrition practice is, how is this working for you? And we can’t know what’s going to work for you unless you tell us. So tell us tell everyone everything and prepare yourself. Not for disappointment.
But arm yourself with the knowledge of you Andrea I don’t even have to say it. You’re literally the most amazing person. I am so grateful you came on today if people want to learn from you or work with you more so learn from you, I know at this point in your career, but can you tell us how they would find you and learn from you?
Andrea Nakayama
Yeah, thank you, Michelle. You can find me at Andrea nakayama.com that will lead you back to the functional nutrition Alliance and the training. They’re back to the clinic there and to any of the work that I’m doing as I continue to build.
Michelle Shapiro
I’m so excited for what you have to come and I know everyone should be waiting with bated breath. Thank you so much, Andre. I love you. Thank you thank you so much for tuning in to the quiet the diet podcast.
If you found any of this information relevant or you related to it, please feel free to share the podcast it would mean the world to us. Also remember to subscribe so you don’t miss any episodes and you can follow us on Instagram at quiet the diet pod. We’ll put the link in the show notes after each episode. Thank you again for listening and I can’t wait to see you in the next episode.
Transcribed by https://otter.ai
Links
Blog Post: Weight Bias in Healthcare
Download the Symptom Tracker
The Functional Nutrition Matrix – image & explanation
Join our FREE membership community!
Andrea Nakayama’s resources:
Andrea’s Website
Functional Nutrition Alliance program
Work with Michelle and her free resources:
Work 1-on-1 with a functional Registered Dietitian at Michelle Shapiro Nutrition LLC
Learn more about the practice
Follow the pod on IG
Follow Michelle on IG
Sign up for the Newsletter